Bemzocaine Dosage Calculator
Bemzocaine is a synthetic amide‑type local anesthetic specifically formulated for oral surgery. It features a rapid onset (under 45seconds), a prolonged duration of action (up to 3hours), and incorporates a proprietary vasoconstrictor blend that minimizes intra‑operative bleeding. The drug received FDA approval in 2021 following extensive phaseIII trials that demonstrated superior analgesia compared with traditional agents.
- Fast onset means less waiting time for patients.
- Extended analgesia reduces the need for re‑injection.
- Vasoconstrictor component cuts down on bleeding and improves visibility.
- Lower systemic toxicity profile enhances safety for high‑risk groups.
- Positive patient feedback translates into better practice reputation.
Mechanism of Action and Key Attributes
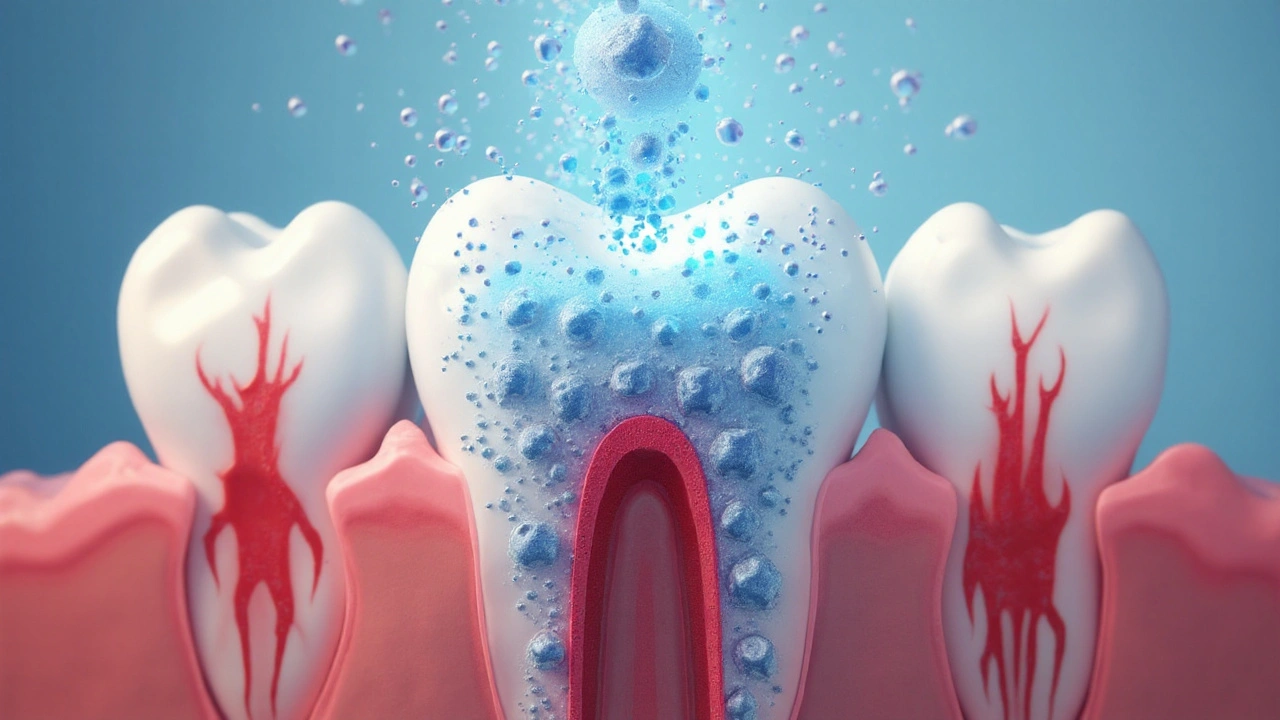
Bemzocaine works by blocking voltage‑gated sodium channels in peripheral nerves, preventing the propagation of pain signals. Its molecular structure includes a lipophilic aromatic ring that facilitates rapid penetration through the mucosal membrane, explaining the swift onset. The built‑in vasoconstrictor-often a combination of epinephrine and a novel peptide-constricts local blood vessels, delaying systemic absorption and extending the anesthetic window.
Clinical Benefits in Common Dental Procedures
From simple extractions to complex endodontic therapy, Bemzocaine delivers consistent numbness across a range of tissues. In crown preparation, the quick onset cuts down chair‑time, allowing the dentist to move from anesthetic injection to drilling in under a minute. For periodontal surgery, reduced bleeding improves the surgeon’s view, decreasing operative time by an estimated 12% according to a 2023 multicenter study involving 1,200 patients.
Patients report lower pain scores on the Visual Analog Scale (VAS) - an average reduction of 2.3 points compared with lidocaine - and a higher willingness to return for future procedures. The longer‑lasting effect also means fewer post‑operative pain spikes, decreasing the prescription of opioid analgesics by roughly 15% in practices that switched to Bemzocaine.
Safety Profile and Contraindications
Bemzocaine’s systemic toxicity threshold (LD50) is 5mg/kg, a full 30% higher margin than lidocaine. This makes it safer for patients with hepatic impairment or low body weight. However, the vasoconstrictor component still warrants caution in patients with uncontrolled hypertension, hyperthyroidism, or certain cardiac arrhythmias.
Adverse reactions are rare. The most common side effects include transient tongue tingling and mild mucosal irritation, typically resolving within 30minutes. A post‑marketing surveillance report from 2024 recorded an overall adverse event rate of 0.08%, well below the 0.2% benchmark for similar agents.
Dosage Guidelines and Administration Tips
Standard adult dosage of Bemzocaine for infiltrative anesthesia is 1.8mL per buccal site, not exceeding 7.2mL per quadrant. For pulp‑test procedures, a 0.9mL supplemental dose can be administered after the initial 30‑second latency period. Always aspirate before injection to avoid intravascular delivery, especially when using the vasoconstrictor‑rich formulation.
When treating pediatric patients, reduce the volume by 30% and watch for signs of anxiety. Using a topical layer of benzocaine prior to injection can further soften the mucosal surface, enhancing patient comfort.
Comparison With Other Popular Dental Anesthetics
| Attribute | Bemzocaine | Lidocaine | Articaine |
|---|---|---|---|
| Onset (seconds) | 45 | 90-120 | 60-80 |
| Duration (hours) | 3+ | 2-3 | 2-2.5 |
| Vasoconstrictor | Mixed peptide‑epinephrine blend | Epinephrine 1:100,000 | Epinephrine 1:100,000 |
| Maximum safe dose (mg/kg) | 7 | 5 | 7 |
| Reported adverse events | 0.08% | 0.15% | 0.12% |
The table shows that Bemzocaine delivers the fastest onset and the longest duration while maintaining a low adverse‑event rate. Its unique vasoconstrictor mix also offers better hemostasis, which is a decisive factor in surgical fields.
Impact on Patient Experience and Practice Efficiency
Patients value speed and comfort. By cutting the waiting period before numbness sets in, dentists can schedule more appointments per day. A dental office in Chicago reported a 9% increase in daily case volume after switching to Bemzocaine, attributing the gain to reduced turnover time between procedures.
From a marketing standpoint, highlighting the use of a cutting‑edge anesthetic can attract anxiety‑prone patients who fear pain. Testimonials often mention "no needle burn" and "quickly back to normal feeling," which are powerful cues for new client acquisition.
Related Concepts and Further Reading
Understanding Bemzocaine’s role fits within the larger framework of dental pharmacology, pain management, and operative dentistry. Readers interested in the biochemical pathways of local anesthetics may explore the sodium channel blockade mechanism in detail. Those focusing on patient safety should review guidelines on vasoconstrictor use in medically compromised populations. Finally, professionals seeking to optimize their workflow can investigate studies on chair‑time reduction linked to rapid‑onset anesthetics.

Frequently Asked Questions
How fast does Bemzocaine take effect?
Patients typically feel numbness within 30-45seconds after injection, allowing the dentist to begin the procedure almost immediately.
Is Bemzocaine safe for children?
Yes, when the dose is reduced by about 30% and proper aspiration techniques are used. Pediatric studies show comparable safety to lidocaine with a smoother onset.
Can patients with hypertension receive Bemzocaine?
Mild to moderate hypertension is generally acceptable, but uncontrolled high blood pressure warrants caution due to the vasoconstrictor component. Always assess the patient’s current medication regimen.
How does Bemzocaine compare cost‑wise to lidocaine?
The per‑vial price is slightly higher (approximately 15% more), but the reduced need for re‑injection and faster turnover often offset the incremental cost.
What are the most common side effects?
Mild tongue tingling and brief mucosal irritation are the most frequently reported. Serious allergic reactions are extremely rare.
Does Bemzocaine reduce the need for post‑operative opioids?
Studies show a 15% drop in opioid prescriptions when dentists adopt Bemzocaine, mainly because patients experience less lingering pain.
Is there a risk of allergy to Bemzocaine?
Allergic reactions are rare; when they occur, they are usually linked to the vasoconstrictor rather than the anesthetic itself. A skin test can be performed if allergy is suspected.
Can Bemzocaine be used for implant surgery?
Yes, its prolonged duration and hemostatic properties make it ideal for multi‑step implant placements where extended anesthesia is beneficial.


Write a comment