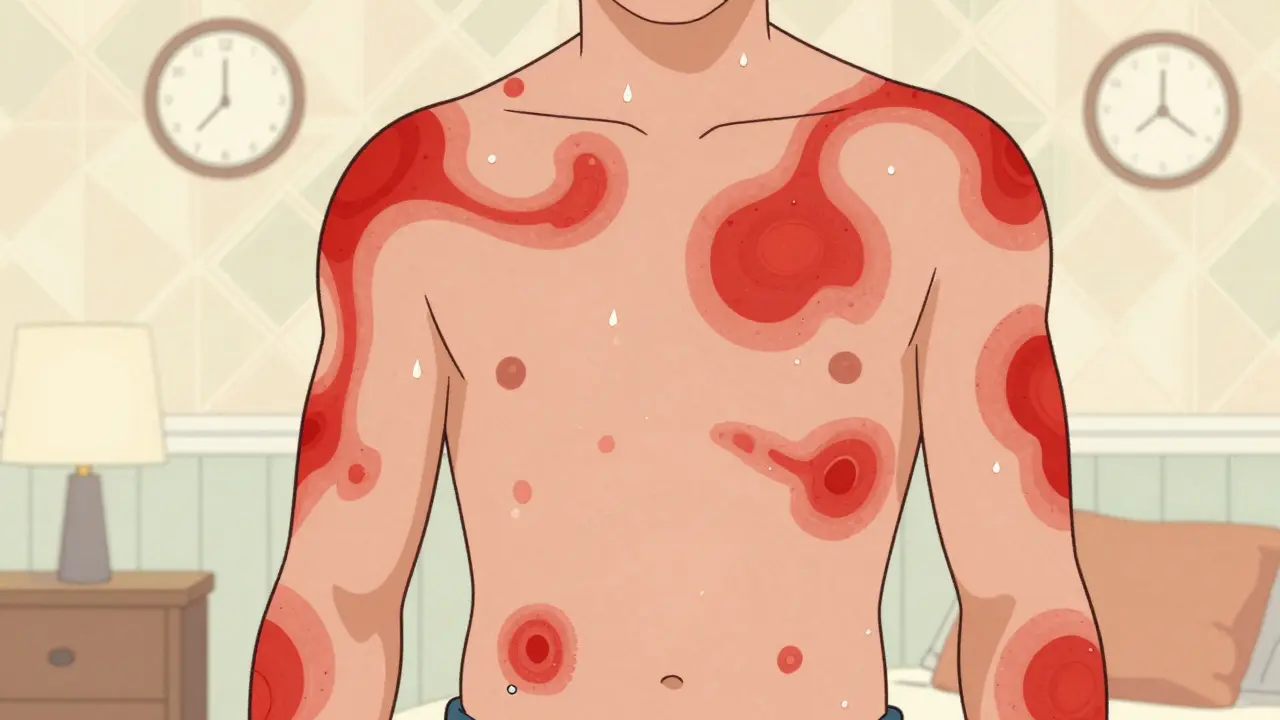
When your skin suddenly breaks out in red, itchy welts that seem to move around your body, it’s not just annoying-it’s unsettling. You might feel like something’s crawling under your skin. That’s urticaria, commonly called hives. It’s not contagious. It’s not usually dangerous. But for millions of people, it’s a daily battle that disrupts sleep, work, and confidence. About 20% of people will get hives at least once in their life. For some, it’s a one-time event. For others, it’s a chronic condition that lasts months or even years.
What Hives Actually Look Like and How They Form
Hives aren’t just a rash. They’re raised, red or skin-colored welts that can be as small as a pinhead or as large as a dinner plate. They often have a pale center and a red border. The itch is intense-not the kind that makes you scratch once or twice, but the kind that makes you want to rub your skin raw. And they don’t stay put. One hive might vanish in an hour, only for another to appear elsewhere. That’s because hives aren’t caused by something sitting on your skin. They’re caused by histamine, a chemical your body releases from mast cells deep in the skin.
When something triggers your immune system-whether it’s food, stress, heat, or nothing obvious at all-those mast cells burst open and dump histamine into the surrounding tissue. Histamine makes tiny blood vessels leak fluid. That fluid swells the skin, creating the raised welt. It also activates nerve endings, causing the itch. This whole process happens in minutes. That’s why hives can appear and disappear so quickly. If the same hive stays in one spot for more than 24 hours, it’s probably not hives. That’s something else, like vasculitis, and needs different testing.
Common Triggers: Food, Stress, and the Mystery of No Cause
People often assume hives are always from food allergies. Peanuts, shellfish, eggs-those are classic triggers. And yes, they can cause hives. But for most people with chronic hives, food isn’t the culprit. In fact, less than 10% of chronic cases are linked to specific foods. More common triggers include:
- Physical stimuli: Heat, cold, pressure, sweat, or sunlight. If you get hives after a hot shower or when your belt digs into your waist, you likely have physical urticaria.
- Medications: Antibiotics like penicillin, NSAIDs like ibuprofen, and even aspirin can trigger outbreaks.
- Infections: Viral infections like colds or stomach bugs are common triggers, especially in kids.
- Stress: Emotional stress doesn’t cause hives directly, but it can make them worse or trigger flares in people who already have them.
- Autoimmune activity: In 30-40% of chronic spontaneous urticaria cases, your own immune system mistakenly attacks your mast cells. No external trigger. Just your body turning on itself.
That last one is the hardest to deal with. If you’ve had hives for more than six weeks and doctors can’t find a cause, you likely have chronic spontaneous urticaria (CSU). It’s not your fault. It’s not allergies. It’s not something you ate. It’s just how your immune system is behaving right now. And it’s more common than you think-70-80% of chronic cases fall into this category.
Antihistamines: The First Line of Defense
When you go to the doctor with hives, the first thing they’ll hand you is an antihistamine. Not because it’s a cure, but because it’s the most effective, safest, and cheapest way to control symptoms. There are two types: first-generation and second-generation.
First-generation antihistamines like diphenhydramine (Benadryl) work fast. But they cross into your brain and cause drowsiness in 50-70% of users. That’s fine for a one-time flare at night, but not for daily use. You can’t drive, work, or focus after taking them.
Second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) are the go-to. They’re non-sedating, last 24 hours, and are available over the counter. Standard dose for adults is 10mg once daily. But here’s the key point most people don’t know: if one pill doesn’t work, taking two might.
The 2021 EAACI/GA²LEN guidelines recommend increasing the dose up to four times the standard amount before moving to stronger treatments. In practice, that means taking 20mg of cetirizine or 30mg of fexofenadine daily. About 40-50% of people with chronic hives get complete control this way. It’s not magic, but it’s science-backed. And it’s safe for long-term use.

When Antihistamines Aren’t Enough
Half of chronic hives patients don’t respond fully to even high-dose antihistamines. That’s when you need to think beyond the pill.
For years, the only option was omalizumab (Xolair), an injectable biologic originally developed for asthma. It was approved for chronic hives in 2014. It works by targeting IgE, the antibody that triggers mast cells. In clinical trials, it helped 65% of patients who didn’t respond to antihistamines. But it costs about $1,500 per injection every four weeks. And you have to go to the clinic for it.
In September 2023, the FDA approved dupilumab (Dupixent) for chronic hives. It blocks two inflammatory pathways (IL-4 and IL-13) and showed 55% of patients achieved complete symptom control in trials-compared to just 15% on placebo. It’s also an injection, but it’s given every two weeks.
Then came remibrutinib, approved in January 2024. This is the first oral tyrosine kinase inhibitor for hives. You take two pills a day. In trials, 45% of patients had complete symptom control. And because it’s a pill, adherence is better than with injections. Patient adherence rates were 85% compared to 70% for omalizumab. That’s a big deal for people juggling work, family, and appointments.
Corticosteroids like prednisone can shut down hives fast. But they’re not a long-term solution. After just three days, 35% of users develop high blood sugar. 25% get insomnia. 20% report mood swings. Most doctors limit them to 3-5 days. Cyclosporine is another option, but it can damage your kidneys and raise blood pressure. These are last-resort drugs for severe, treatment-resistant cases.
Real People, Real Experiences
Online communities like Reddit’s r/ChronicHives have over 15,000 members. In a 2023 survey of 1,245 people there, 68% said hives ruined their sleep. Over 40% woke up 2-3 times a night from itching. One user wrote: “Cetirizine gives me 8-10 hours of relief. I take it at 7 p.m. and wake up without a single welt.” Another: “Loratadine barely lasts 6 hours. I’m taking it three times a day just to feel normal.”
People on PatientsLikeMe who use omalizumab report 72% satisfaction. “Complete control in four weeks,” one wrote. But 35% said the injections hurt and left bruises. Prednisone got brutal reviews: “I was crying, angry, and couldn’t sleep. I’d rather have the hives.”
And then there’s the diagnosis delay. Over 20% of chronic hives patients saw three or more doctors before getting the right diagnosis. That’s not because doctors are careless. It’s because hives look like so many other things. And chronic spontaneous urticaria doesn’t show up on blood tests. It’s a diagnosis of exclusion.

How to Get Started: A Simple Plan
You don’t need a specialist to begin managing hives. Here’s what works for most people:
- Start with a second-generation antihistamine. Cetirizine 10mg daily. Take it at the same time each day. Don’t wait until you break out.
- Keep a symptom diary. Note what you ate, where you were, how stressed you felt, what you wore, and how the hives changed. Look for patterns over 2-4 weeks.
- If no improvement in two weeks, double the dose. Try 20mg of cetirizine or 180mg of fexofenadine. Give it two more weeks.
- If still not controlled, see an allergist. They’ll check for physical triggers, autoimmune markers, and discuss biologics if needed.
Some people find that combining a non-sedating antihistamine in the morning with a low-dose sedating one at night helps with sleep and overall control. Studies show this combo improves symptom control by 30%.
What to Avoid
Don’t assume your hives are from food unless you’ve clearly linked them to a specific meal-within minutes or hours-and it happens every time. Elimination diets can be stressful and often unnecessary.
Don’t use steroid creams on hives. They don’t work. The problem is under the skin, not on top of it.
Don’t ignore mental health. The European Academy of Dermatology found that 15-20% of chronic hives patients develop anxiety or depression. The constant itch, the unpredictability, the sleep loss-it wears you down. Talk to someone. Therapy helps.
The Future: Personalized Treatment and Better Access
The treatment landscape is changing fast. New oral drugs like remibrutinib are making daily life easier. By 2030, experts predict a 15% rise in chronic hives cases due to environmental changes and increased immune sensitivity. But there’s a gap. In low-income countries, only 30% of patients can access biologics. In high-income countries, it’s 85%. That’s not fair.
Telemedicine is helping. Nearly half of allergists now use video visits for hives management. That means you don’t need to drive hours to see a specialist. Apps like Urticaria Tracker let you log symptoms, triggers, and medication timing. They’re not perfect, but they’re better than paper diaries.
Down the road, genetic testing might tell you which antihistamine your body responds to best. Some people metabolize cetirizine slowly. Others clear it too fast. That’s why one person feels great on 10mg and another needs 40mg. Personalized dosing is coming. It’s not science fiction-it’s already being tested in labs.

Write a comment