Skin Infection & Pain Assessment Tool
Assess Your Symptoms
This tool helps you recognize potential skin infection signs. It's not a diagnosis but can guide when to seek professional care.
Pain Assessment
Infection Signs
Risk Level
When Skin Pain is discomfort, burning, or aching that originates from the skin's surface or deeper layers, it can signal anything from a minor irritation to a serious infection. Pair that with Skin Infection (the invasion of microorganisms that cause inflammation and tissue damage), and you’ve got a health issue that deserves attention.
What Triggers Skin Pain?
Skin pain doesn’t always come with a rash or visible lesion. Common triggers include:
- Mechanical injury - cuts, scrapes, or burns that damage nerve endings.
- Inflammatory skin disorders - eczema or psoriasis flare‑ups can make the skin hypersensitive.
- Infections - bacterial, viral, or fungal agents release toxins that irritate the skin.
- Systemic conditions - diabetes or peripheral neuropathy sometimes manifest as foot or leg skin pain.
Identifying the root cause is the first step toward relief.
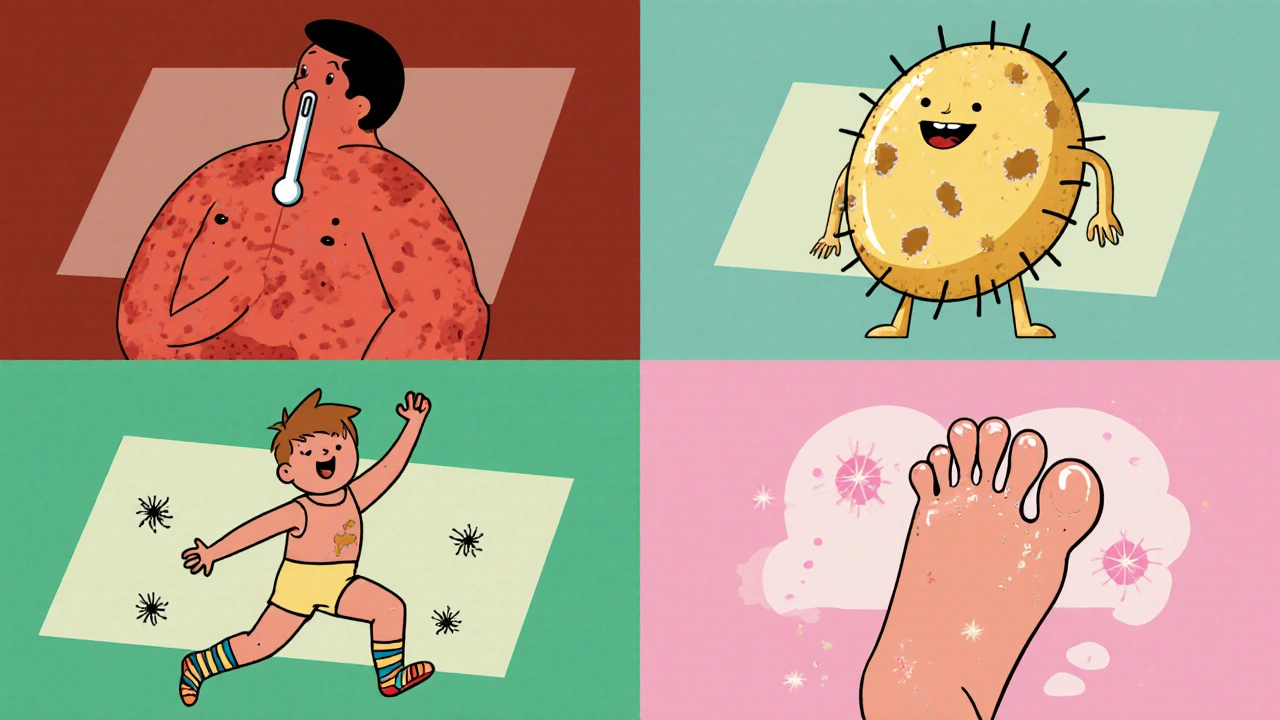
Common Types of Skin Infections
Not all skin infections look alike. Below are the most frequently encountered ones.
| Infection | Primary Cause | Typical Symptoms | First‑Line Treatment |
|---|---|---|---|
| Cellulitis | Staphylococcus aureus or Streptococcus pyogenes | Red, warm, tender area; fever; swelling | Oral antibiotics (e.g., cephalexin) |
| Impetigo | Staphylococcus aureus (often MRSA) or Streptococcus | Honey‑colored crusts, itchy lesions, usually on face or arms | Topical mupirocin or oral antibiotics if extensive |
| Fungal Infection (e.g., athlete’s foot) | Dermatophytes such as Trichophyton rubrum | Itching, scaling, and red borders, often between toes | Topical antifungals (clotrimazole, terbinafine) |
| Herpes Simplex Virus (cold‑sores, genital herpes) | HSV‑1 or HSV‑2 virus | Painful blisters that rupture, tingling before breakout | Antiviral meds (acyclovir) for outbreaks |
How to Spot the Difference Between Pain and Infection
Both pain and infection can coexist, but certain clues point to one or the other:
- Pain alone: Usually sharp, localized, and improves with rest or topical analgesics.
- Infection signs: Redness spreading beyond the original spot, warmth, pus, fever, or swollen lymph nodes.
- Combined symptoms: When a cut becomes red, swollen, and painful, think infection.
If you notice any systemic symptoms-fever above 38°C (100.4°F), chills, or unexplained fatigue-seek medical help immediately.
When to Seek Professional Care
Self‑care works for minor irritations, but here’s when you should call a clinician:
- Rapidly spreading redness or swelling.
- Pain that worsens despite over‑the‑counter remedies.
- Presence of pus, foul odor, or open sores that don’t close.
- Fever, chills, or feeling generally unwell.
- Underlying health issues - diabetes, immune suppression, or peripheral vascular disease.
Early treatment can prevent complications like abscess formation or sepsis.
Prevention Strategies to Keep Skin Pain and Infections at Bay
Most skin troubles are preventable with simple habits:
- Maintain clean skin: Wash daily with mild soap, especially after sweating.
- Moisturize regularly: Dry skin cracks become entry points for microbes.
- Protect cuts: Apply sterile dressings and change them daily.
- Avoid sharing personal items: Towels, razors, and footwear can spread fungi and bacteria.
- Choose breathable footwear: Tight shoes encourage moisture buildup, perfect for fungi.
- Manage chronic conditions: Keep blood sugar stable if you have diabetes.
Even if you’re active outdoors, a quick shower and clean clothes afterward can make a huge difference.

Treatment Options: From Home Remedies to Prescription Meds
Depending on severity, treatment ranges from simple home care to prescription medication.
Home Care for Minor Pain
- Cool compresses for 10‑15 minutes to soothe burning.
- Over‑the‑counter (OTC) analgesics such as ibuprofen (200‑400 mg every 6 hours) for inflammation.
- Topical lidocaine gels for temporary numbing.
OTC Antiseptics and Antifungals
For small cuts or suspected fungal patches, products like bacitracin ointment or clotrimazole cream are effective.
Prescription Antibiotics
If a bacterial infection is confirmed, a doctor may prescribe oral antibiotics (e.g., doxycycline for cellulitis) or topical agents. Complete the full course, even if symptoms improve early.
Antiviral Therapy
For HSV outbreaks, antivirals taken at the first sign of tingling can shorten duration and lessen pain.
When Surgery Is Needed
Abscesses that don’t drain on their own often require incision and drainage in a clinical setting.
Never self‑prescribe strong antibiotics or steroids; misuse can worsen infections or mask warning signs.
Quick Reference Checklist
- Assess pain intensity and any accompanying redness or swelling.
- Check for systemic symptoms - fever, chills, malaise.
- Apply appropriate home care (clean, cool, OTC pain relief).
- Use targeted OTC creams for suspected fungal or bacterial spots.
- Seek medical care if symptoms spread, worsen, or include fever.
- Follow prescribed medication regimens exactly as directed.
- Practice daily skin hygiene and protect any breaks.
Can stress cause skin pain?
Yes. Stress releases cortisol and inflammatory mediators that can amplify pain perception and trigger flare‑ups of conditions like eczema, making the skin feel sore or itchy.
How long does cellulitis take to heal with antibiotics?
Most uncomplicated cases improve within 48‑72 hours and resolve fully after a 7‑10 day course of oral antibiotics, provided the infection is caught early.
Is it safe to use over‑the‑counter creams on open wounds?
Generally avoid creams that aren’t labeled for open wounds. Antiseptic ointments like bacitracin are safe, but moisturizers or fragrance‑filled lotions can irritate the area.
What’s the difference between a rash and an infection?
A rash is a skin reaction that may be allergic, autoimmune, or irritant without microbes. An infection involves bacteria, viruses, or fungi actively invading tissue, often with pus, fever, or spreading redness.
Can diabetes increase the risk of skin infections?
Yes. High blood sugar impairs immune response and reduces circulation, making cuts heal slower and providing a fertile environment for bacteria and fungi.


Write a comment