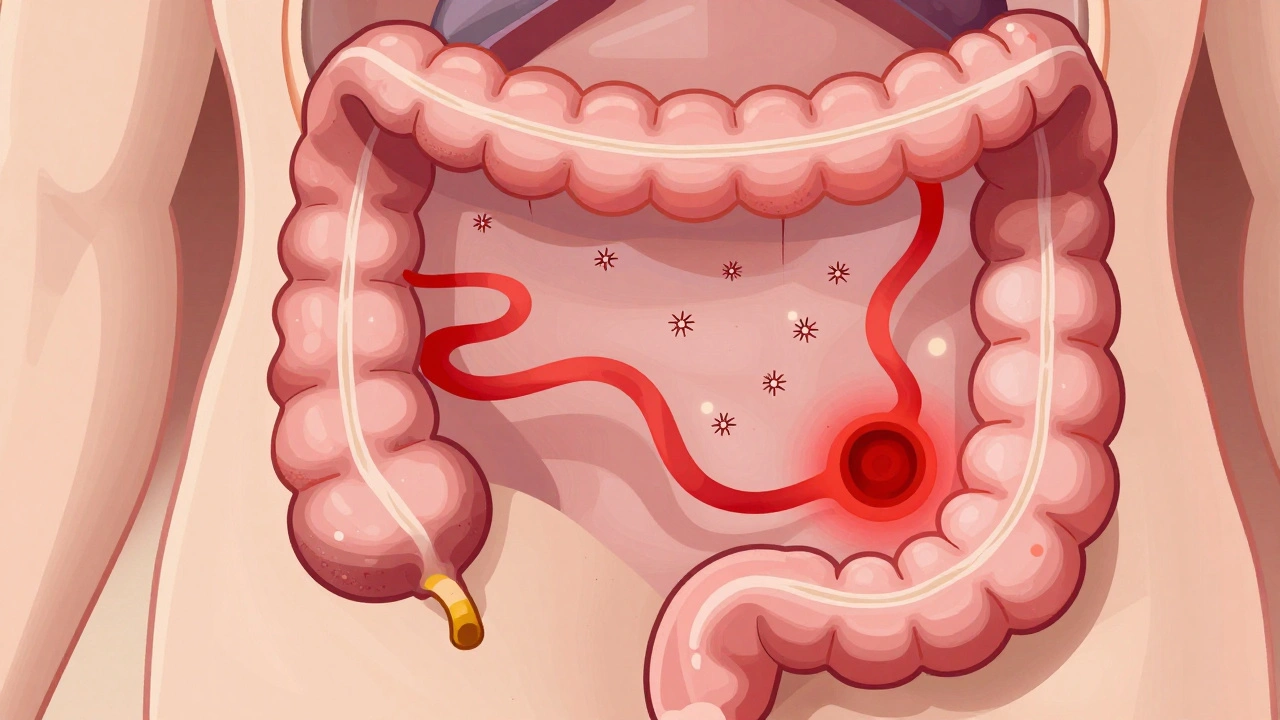
Ulcerative colitis isn’t just frequent diarrhea or occasional stomach cramps. It’s a lifelong condition where the inner lining of your colon and rectum becomes chronically inflamed, forming open sores that bleed and cause pain. Unlike a stomach bug that fades in a few days, ulcerative colitis (UC) flares up unpredictably-sometimes after months of calm, sometimes without warning. The good news? Most people with UC can live full, active lives. But that only happens when you understand what’s really going on inside your body-and how to stop the inflammation before it takes over.
What Exactly Happens in Your Colon With Ulcerative Colitis?
- Your colon’s inner lining gets attacked by your own immune system.
- This triggers swelling, ulcers, and constant irritation.
- The damage doesn’t skip areas-it spreads continuously from the rectum upward.
- Unlike Crohn’s disease, UC never digs through all layers of the bowel wall.
The inflammation causes the colon to empty too often and too urgently. You might feel the need to go every 10 minutes-and still feel like you haven’t emptied completely. That’s called tenesmus. Blood and mucus mix with stool, sometimes turning it into a watery red sludge. In severe cases, people have more than 10 bowel movements a day. Nighttime cramps are common. Sleep? Often gone.
The Five Types of Ulcerative Colitis (And What They Mean for You)
Not all UC is the same. Where the inflammation stops tells doctors how serious it is-and what kind of treatment you’ll need.- Ulcerative proctitis: Only the rectum is affected. Symptoms? Mostly rectal bleeding and urgency. This is the mildest form. Cancer risk is low.
- Proctosigmoiditis: Inflammation reaches the sigmoid colon (the S-shaped lower part). You’ll notice more frequent bloody diarrhea and cramping on the lower left side.
- Left-sided colitis: The inflammation goes up to the splenic flexure (near the spleen). Pain shifts to the left abdomen. Weight loss and loss of appetite become common.
- Pancolitis: The entire colon is inflamed. This is the most severe form. Symptoms include severe bloody diarrhea, fever, extreme fatigue, and rapid weight loss. Cancer risk is higher here.
- Rectal-sparing UC: Rare. The rectum stays healthy, but the rest of the colon is damaged. Symptoms mirror pancolitis but without rectal bleeding.
Knowing your type helps predict what’s coming. Someone with ulcerative proctitis might manage with a daily suppository. Someone with pancolitis may need biologic drugs or even surgery.
What Triggers a Flare-Up? (And What Doesn’t)
People often blame stress or spicy food for causing UC. They don’t. The root cause is your immune system going rogue. But triggers? Those are real.- Stress: Not the cause-but it can turn a quiet colon into a storm. High-stress events (job loss, grief, surgery) often precede flares.
- Antibiotics: Can disrupt gut bacteria, leading to inflammation spikes.
- Nonsteroidal anti-inflammatories (NSAIDs): Ibuprofen, naproxen-even aspirin-can irritate the colon lining.
- Some foods: Dairy, high-fat meals, caffeine, alcohol, and raw veggies can worsen symptoms during flares. Not because they cause UC, but because inflamed tissue can’t handle them well.
Here’s what doesn’t trigger UC: your diet before diagnosis, childhood eating habits, or eating too much sugar. You didn’t do anything wrong to get this. And you can’t fix it by eating kale or taking probiotics alone.
Extra-Intestinal Symptoms: It’s Not Just Your Gut
UC doesn’t stay in the colon. About one in three people with UC experience symptoms elsewhere:- Red, itchy, burning eyes (uveitis or episcleritis)
- Joint pain in knees, ankles, or wrists-sometimes worse than gut pain
- Red, tender lumps under the skin (erythema nodosum)
- Painful mouth sores
- Nausea and vomiting during severe flares
These aren’t random. They’re signs your immune system is overactive everywhere. Treating the colon often helps these too. But sometimes, you need separate treatments-like arthritis meds for joint pain.
How Doctors Treat Ulcerative Colitis
Treatment isn’t one-size-fits-all. It’s a ladder. You start at the bottom and climb up only if you need to.- Aminosalicylates (5-ASAs): Mesalamine, sulfasalazine. Used for mild to moderate UC. Taken as pills, suppositories, or enemas. They reduce inflammation directly in the colon lining.
- Corticosteroids: Prednisone or budesonide. Fast-acting for flares-but not for long-term use. Side effects include weight gain, mood swings, and bone thinning.
- Immunomodulators: Azathioprine, 6-MP. These calm your immune system over months. Used when 5-ASAs aren’t enough. Takes 3-6 months to work.
- Biologics: Infliximab, adalimumab, vedolizumab. Injected or infused. Target specific immune proteins causing inflammation. Many people achieve remission with these.
- JAK inhibitors: Tofacitinib. Newer oral pills that block inflammation signals inside cells.
- Colectomy: Surgery to remove the colon. The only cure for UC. Done when medications fail, cancer risk is high, or bleeding becomes life-threatening.
Biologics changed everything. Ten years ago, many people with moderate UC ended up needing surgery. Now, many stay on these drugs for years-and stay in remission. Some even stop having symptoms entirely.
Getting Into and Staying in Remission
Remission doesn’t mean you’re cured. It means no active inflammation, no bleeding, no urgent bowel movements. You feel normal. But the disease is still there-sleeping.To stay in remission:
- Take your meds-even when you feel fine. Stopping medication is the #1 reason flares return.
- Get regular colonoscopies. Every 1-2 years if you’ve had UC for 8+ years. This screens for early signs of colon cancer, which is higher in pancolitis.
- Track your symptoms. Use a journal or app. Note food, stress, sleep, bowel habits. Patterns emerge over time.
- Don’t ignore extra-intestinal symptoms. Joint pain or eye redness? Tell your doctor. It’s a sign your immune system is still active.
- Build a support system. UC is isolating. Talking to others who get it-online or in person-makes a huge difference.
Some people find that low-FODMAP diets help during flares. Others do better with a low-residue diet. There’s no universal diet. But keeping a food-symptom log helps you find your personal triggers.

What Life Looks Like After Diagnosis
I’ve met people with UC who run marathons. I’ve met others who work full-time from home because they can’t risk being far from a bathroom. Both are valid.What matters isn’t how bad your symptoms are today. It’s whether you have a plan. A plan means:
- Knowing your type of UC
- Having a treatment strategy with your doctor
- Understanding your triggers
- Carrying emergency supplies (wipes, change of clothes, medication)
- Not letting fear control your life
Most people with UC live full lives. They travel. They have kids. They work. They laugh. But they do it with a map. Without one, the disease wins. With one, you take back control.
When to Call Your Doctor Immediately
Not every flare needs an ER visit. But these signs do:- More than 10 bloody bowel movements a day
- Fever over 101°F (38.3°C) that won’t go down
- Severe abdominal pain or swelling
- Vomiting blood or black, tarry stools
- Feeling dizzy, faint, or heart racing
These could mean toxic megacolon-a rare but life-threatening complication where the colon swells dangerously. Don’t wait. Go to the hospital.
Can ulcerative colitis be cured?
The only cure for ulcerative colitis is surgical removal of the entire colon and rectum (colectomy). After this surgery, UC cannot return. However, most people manage their condition with medication and live without symptoms for years. Remission is the goal-not necessarily a cure.
Does stress cause ulcerative colitis?
No. Stress doesn’t cause ulcerative colitis. The disease is caused by an abnormal immune response. But stress can trigger a flare-up in people who already have UC. Managing stress through sleep, exercise, or therapy can help reduce flare frequency.
Is ulcerative colitis the same as Crohn’s disease?
No. Both are types of inflammatory bowel disease, but they’re different. Ulcerative colitis only affects the inner lining of the colon and rectum, with continuous inflammation. Crohn’s disease can affect any part of the digestive tract, involves deeper tissue layers, and causes patchy areas of damage with healthy tissue in between.
Can I still eat normally with ulcerative colitis?
Yes-but not always. During flares, high-fiber, spicy, fatty, or dairy-heavy foods can make symptoms worse. Many people do better with low-residue or low-FODMAP diets during active disease. When in remission, most can return to a normal diet. Individual triggers vary, so tracking what you eat and how you feel helps you personalize your plan.
Do I need a colonoscopy every year if I have UC?
Not every year. If you’ve had UC for 8 years or more, especially if it affects your whole colon, you should have a colonoscopy every 1-2 years to check for precancerous changes. If your disease is limited to the rectum, screening may be less frequent. Your doctor will recommend a schedule based on your type, duration, and family history.
Are biologic drugs safe for long-term use?
Biologics are generally safe for long-term use in most people with UC. They work by targeting specific parts of the immune system that cause inflammation. Risks include increased chance of infections and, rarely, certain cancers. But for many, the benefit of staying in remission outweighs the risks. Your doctor will monitor you with blood tests and screenings.
Next Steps: What to Do Today
If you’ve been diagnosed with UC:- Write down your type of UC and what parts of your colon are affected.
- Ask your doctor: “What’s my treatment plan if this flare doesn’t improve in 2 weeks?”
- Start a symptom journal-note bowel frequency, pain level, food, and stress.
- Find a support group-even online. You’re not alone.
- Don’t skip your next colonoscopy. It’s not about punishment. It’s about prevention.
If you think you might have UC-bloody diarrhea, cramps, urgency that won’t go away-don’t wait. See a gastroenterologist. Early diagnosis means early control. And early control means more years of feeling like yourself.

Write a comment