Anticholinergic Burden Calculator
Medication Risk Assessment
This tool helps you calculate the cumulative anticholinergic burden of your medications. A score of 4 or higher indicates high risk of cognitive impairment and delirium.
Current Medications
Anticholinergic Burden Score
What Your Score Means
0-1: Low risk of anticholinergic effects
2-3: Moderate risk of cognitive impairment over time
4+: High risk - increases risk of delirium, confusion, and dementia
Warning: A score of 4 or higher indicates high risk of cognitive impairment and delirium. This combination may cause confusion, memory problems, and urinary retention. Consider speaking with your healthcare provider about safer alternatives.
Safer Alternatives
Consider these alternatives to reduce anticholinergic burden:
- Allergies: Loratadine, fexofenadine, or cetirizine (ACB score of 0)
- Sleep: Melatonin instead of diphenhydramine
- Depression/Pain: Nortriptyline, sertraline, gabapentin, or pregabalin
- Note: Always consult your healthcare provider before changing medications
Combining tricyclic antidepressants (TCAs) with common over-the-counter antihistamines like diphenhydramine (Benadryl) might seem harmless - especially if you're trying to sleep better or manage allergies. But for many people, especially those over 65, this combo can trigger something dangerous: anticholinergic overload. It’s not rare. It’s not theoretical. It’s happening in clinics and ERs right now, often because no one connected the dots between two widely prescribed or self-administered drugs.
What Is Anticholinergic Overload?
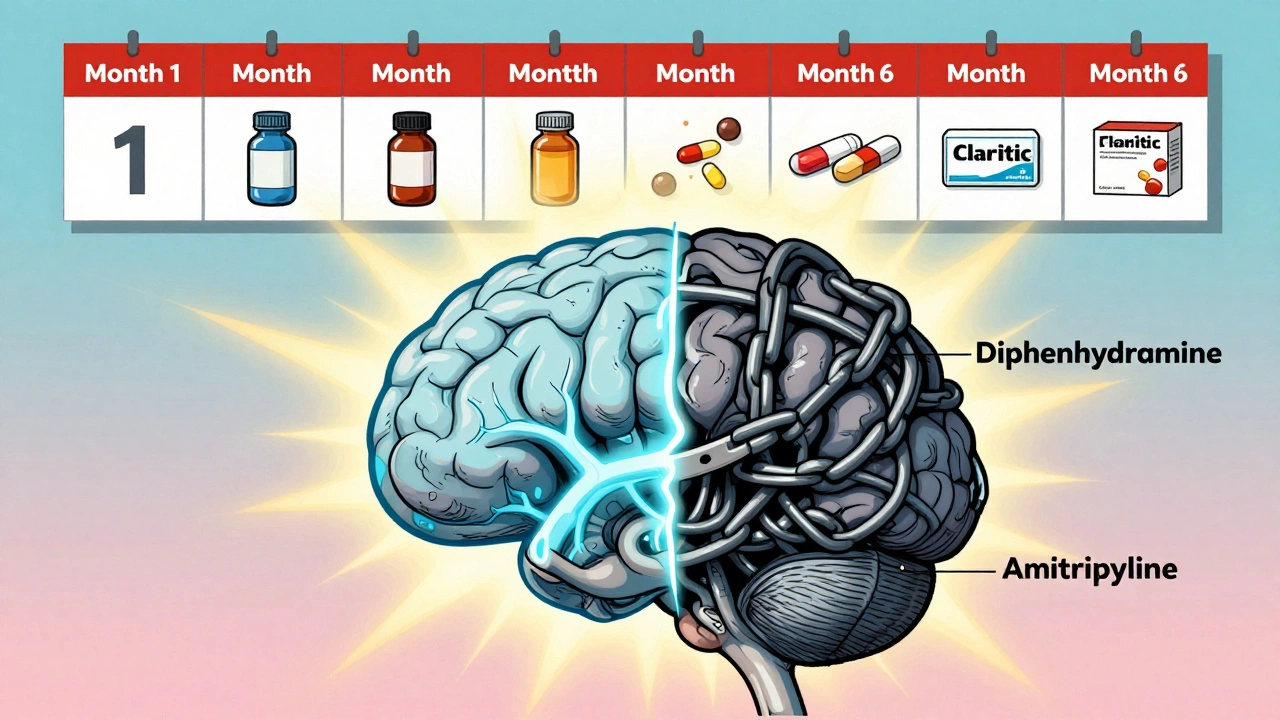
Your body uses acetylcholine to control everything from memory and attention to bladder function and heart rate. Anticholinergic drugs block this chemical. A single drug with mild anticholinergic effects might cause dry mouth or drowsiness. But when you stack multiple drugs that do the same thing - like a TCA and a first-gen antihistamine - your brain and body get overwhelmed. That’s anticholinergic overload.It doesn’t take much. Amitriptyline, a common TCA, scores a 3 on the Anticholinergic Cognitive Burden (ACB) scale - the highest possible. Diphenhydramine scores a 2. Together? That’s a 5. Research shows that a cumulative ACB score of 4 or higher doubles your risk of dementia over time. For older adults, this isn’t just a side effect - it’s a slow-motion neurological crisis.
Why TCAs and Antihistamines Are a Perfect Storm
Tricyclic antidepressants like amitriptyline, imipramine, and clomipramine were designed in the 1950s to treat depression. They work by boosting serotonin and norepinephrine. But they also block muscarinic receptors - the same ones targeted by anticholinergic drugs. That’s why TCAs cause constipation, blurred vision, urinary retention, and confusion. These aren’t side effects you can ignore. They’re signs your nervous system is drowning in blocked signals.First-generation antihistamines like diphenhydramine and hydroxyzine were made to stop allergies. But they cross the blood-brain barrier easily and hit those same muscarinic receptors. That’s why Benadryl makes you sleepy - and why, when paired with a TCA, it can turn mild forgetfulness into full-blown delirium.
Here’s the math: A 72-year-old on 50 mg of amitriptyline for nerve pain takes 25 mg of diphenhydramine at night for sleep. Both drugs are metabolized by the same liver enzyme (CYP2D6). If the patient is a slow metabolizer - which about 7% of people are - levels build up fast. Blood concentrations of amitriptyline can spike past the safe range of 300 ng/mL. That’s when you see confusion, hallucinations, rapid heartbeat, and urinary retention. One 2020 study found over 3,300 patients flagged for this exact combination in electronic health records.
Who’s at Risk - And Why It’s Often Missed
Elderly patients are the most vulnerable. Their kidneys and liver don’t clear drugs as efficiently. Their brains have fewer acetylcholine receptors to begin with. But the problem isn’t just age. It’s prescribing habits.Primary care doctors still prescribe diphenhydramine for insomnia because it’s cheap, available, and seems harmless. They know TCAs cause side effects - but rarely calculate the total anticholinergic load. A 2023 survey found that 78% of psychiatrists now check ACB scores, but only 32% of primary care providers do. That gap is deadly.
One patient in Vancouver, 78, was on amitriptyline for diabetic neuropathy. His family doctor added Benadryl for “trouble sleeping.” Within two weeks, he was disoriented, couldn’t urinate, and was hospitalized. His ACB score was 5. He’d been on both drugs for less than a month. He didn’t have dementia before. He developed anticholinergic delirium - reversible, but terrifying.
It’s not just older adults. People with chronic pain, depression, or anxiety are often on multiple meds. A 2022 JAMIA study showed that 92% of EHR systems now flag TCA-antihistamine combos - but many still get approved because the prescriber clicks past the alert. The system warns, but the human doesn’t listen.

What Alternatives Actually Work?
You don’t have to suffer through poor sleep or allergies just to avoid a dangerous combo. There are safer choices.- For allergies: Switch from diphenhydramine to loratadine (Claritin), fexofenadine (Allegra), or cetirizine (Zyrtec). These second-gen antihistamines have an ACB score of 0. They don’t cross into the brain. No confusion. No dry mouth. Just relief.
- For sleep: Melatonin (0.5-5 mg) works better than diphenhydramine for long-term use. It doesn’t block acetylcholine. It helps regulate your natural sleep cycle. A 2023 study in the Journal of the American Geriatrics Society showed that replacing anticholinergic sleep aids with melatonin reduced cognitive decline by 34% in six months.
- For depression or pain: If you’re on amitriptyline and struggling with side effects, ask about nortriptyline or desipramine. They’re still TCAs, but with lower anticholinergic activity. Or consider an SSRI like sertraline - which has a 0 ACB score - for depression. For pain, gabapentin or pregabalin are often better tolerated.
Some patients worry that switching meds means losing effectiveness. But for neuropathic pain, amitriptyline works - but so do other options. A 2021 Cochrane review found that gabapentin and duloxetine were just as effective for nerve pain, with far fewer cognitive risks.
The Real Cost of Ignoring This Interaction
The damage isn’t just physical. It’s financial, emotional, and systemic.A single hospitalization for anticholinergic delirium can cost over $15,000. The average length of stay? Five days. Many patients never fully recover their mental sharpness. A 2015 JAMA Internal Medicine study found that people who took high-burden anticholinergics for more than three years had a 54% higher risk of dementia. That’s not a small increase. That’s a major public health threat.
And it’s preventable. The American Geriatrics Society’s Beers Criteria (2023) says clearly: “Avoid first-generation antihistamines in older adults taking TCAs.” Yet, a 2021 survey found that 28% of monthly anticholinergic overload cases involved exactly this combo. That’s not ignorance - it’s inertia.
Pharmacists are seeing it. One pharmacist in Calgary told me she caught 12 such combinations in a single month. She called the prescribers. Ten changed the script. Two didn’t. One of those two patients ended up in the ER.
What You Can Do Today
If you’re taking a TCA - amitriptyline, nortriptyline, imipramine - and you’re also using diphenhydramine, hydroxyzine, or any OTC sleep or allergy aid:- Check your ACB score. Amitriptyline = 3. Diphenhydramine = 2. Add them. If it’s 4 or higher, you’re at risk.
- Ask your doctor or pharmacist to review all your meds. Include supplements, OTC drugs, and herbal products. Even some cough syrups contain anticholinergics.
- Ask for alternatives. “Is there a non-sedating antihistamine I can use instead?” “Can we try melatonin for sleep?”
- Track your symptoms. Are you forgetting names? Having trouble finding words? Feeling unusually foggy? Urinating less? These aren’t normal aging - they’re red flags.
You don’t need to stop your TCA. You don’t need to suffer. You just need to know the risk - and speak up.
What’s Changing - And Why It Matters
The tide is turning. In 2023, the FDA required all TCA and first-gen antihistamine labels to include warnings about cumulative anticholinergic effects. Electronic health records now block these combinations unless overridden - and many hospitals require a pharmacist sign-off.Research is accelerating too. The National Institute on Aging is funding a $2.4 million study to track how even short-term exposure (30 days) to these combos affects cognition in seniors. Early data shows a 200% spike in delirium risk.
And the most hopeful part? Deprescribing works. When patients stop high-burden anticholinergics, their brains bounce back. A 2023 study found that after six months off these drugs, 60% of elderly patients showed measurable improvement in memory and attention. It’s not a cure - but it’s a recovery.
This isn’t about avoiding medication. It’s about using it wisely. You can manage pain. You can sleep. You can breathe easier. You just need to make sure you’re not poisoning your brain in the process.

Write a comment