Statin Myopathy Risk Calculator
This tool helps you assess your risk of developing statin-related muscle pain based on factors discussed in the article. It's not a substitute for medical advice, but can help guide discussions with your healthcare provider.
Your Statin Myopathy Risk
Recommendations
This tool is based on clinical research and provides an estimated risk assessment. It should not replace professional medical advice. Always discuss your individual situation with your healthcare provider.
For millions of people taking statins to lower cholesterol, muscle pain isn’t just a nuisance-it can be a dealbreaker. Around 10-30% of statin users report muscle discomfort, weakness, or cramps, and for many, it leads to stopping the medication altogether. But here’s the catch: not all muscle pain from statins is the same. Some is mild and temporary. Others are signs of a deeper biological disruption-what doctors now call statin-induced myopathy. This isn’t just a side effect. It’s a cascade of molecular events inside your muscle cells that can turn a routine prescription into a serious health dilemma.
What’s Really Happening in Your Muscles?
Statins work by blocking HMG CoA reductase, an enzyme in the liver that makes cholesterol. But that same enzyme is also involved in making other vital molecules-like CoQ10 and isoprenoids-that your muscles need to function properly. When statins cut off these building blocks, things start to go wrong at the cellular level.
One key discovery from a 2019 study in the Journal of the American College of Cardiology showed that statins cause a protein called FKBP12 to detach from the ryanodine receptor (RyR1) in muscle cells. This receptor controls calcium release. When FKBP12 is gone, calcium leaks out uncontrollably-2.3 times more than normal. That flood of calcium triggers enzymes that break down muscle fibers, leading to pain, fatigue, and weakness. What’s startling is that this happens in skeletal muscle but not heart muscle. That’s why your heart keeps beating fine while your legs feel like lead.
On top of that, statins reduce CoQ10 levels in muscle tissue by about 40% after just four weeks. CoQ10 is essential for energy production in mitochondria-the powerhouses of your cells. Less CoQ10 means less energy, more oxidative stress, and muscle fatigue. Studies show reactive oxygen species increase by 35% in affected muscles, which further damages cells.
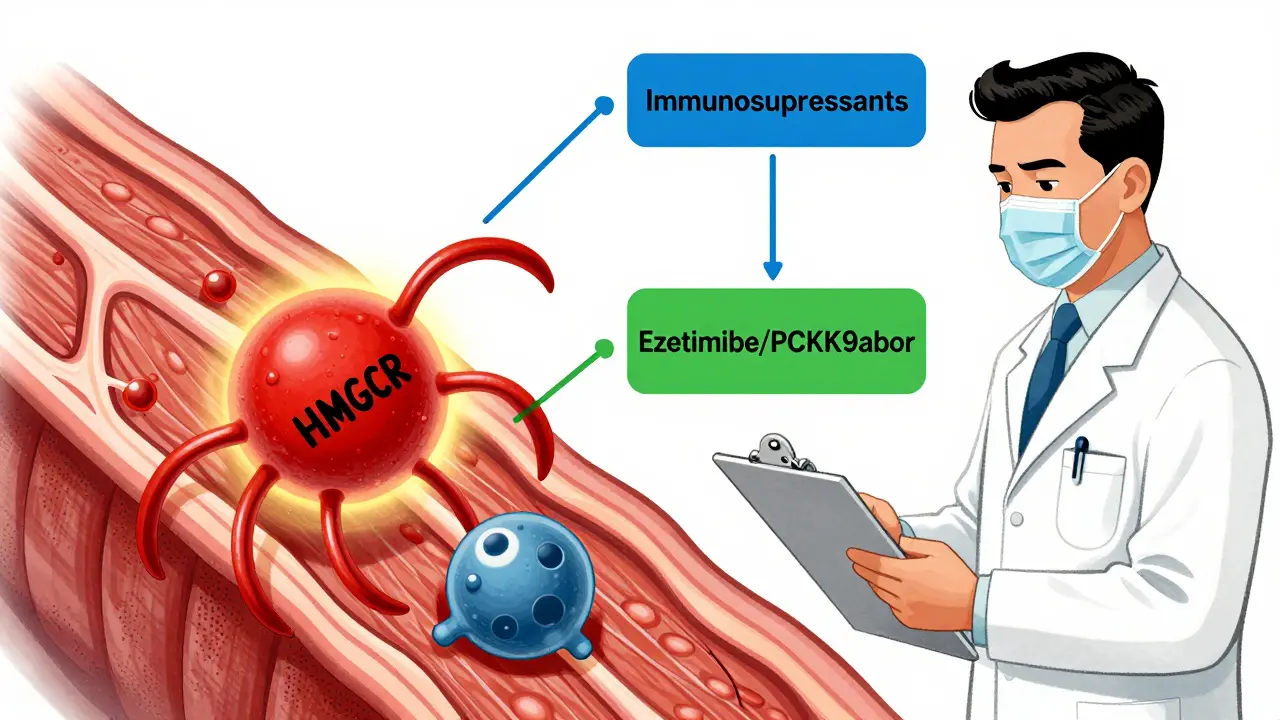
Then there’s the less common but more severe form: autoimmune myopathy. In about 5-10% of persistent cases, the body starts producing antibodies against HMGCR-the very enzyme statins target. These antibodies attack muscle tissue, causing inflammation and severe weakness. This form doesn’t go away when you stop the statin. It often needs immunosuppressants like prednisone and methotrexate to calm the immune response.
Who’s Most at Risk?
Not everyone on statins gets muscle pain. But certain factors raise your risk:
- Age over 65
- Female gender
- Small body frame or low muscle mass
- Chronic kidney or liver disease
- Taking other medications like fibrates, cyclosporine, or certain antibiotics
- Genetic variants in SLCO1B1, a gene that controls how statins enter the liver
- Low vitamin D levels
- Sedentary lifestyle
Interestingly, people who exercise regularly are less likely to develop severe symptoms. A 2021 Mayo Clinic study found that those who maintained 150 minutes of moderate exercise per week had 58% fewer muscle complaints than sedentary users. Exercise seems to help stabilize the RyR1 channel, reducing calcium leaks.
How Do You Know It’s Statins?
Statins don’t always cause muscle pain. Many people feel discomfort and assume it’s the drug-even when it’s not. That’s why doctors use a simple but effective test: the statin washout.
If you stop the statin and your symptoms improve within 1-4 weeks, it’s likely statin-related. If symptoms persist, something else might be going on-like thyroid issues, vitamin D deficiency, or even a different muscle disorder. Rechallenging with the same statin at a lower dose can confirm the link. About 65% of people tolerate a reduced dose after a washout period.
For more certainty, doctors may check creatine kinase (CK) levels. If CK is more than 10 times the upper limit of normal, it’s a clear sign of muscle breakdown. But here’s the twist: many people with statin myopathy have normal CK levels. That’s why symptoms matter more than blood tests.
What Can You Do About It?
Stopping statins isn’t always the answer. For people with high cholesterol and heart disease risk, the benefits often outweigh the risks. The goal isn’t to quit-it’s to manage.
CoQ10 supplementation is one of the most studied options. A 2022 European study found that 200 mg per day reduced muscle pain in 35% of patients. While not a cure-all, it helps enough that many doctors now recommend it as a first step.
Exercise is another powerful tool. A 2023 phase II trial showed that combining 150 minutes of weekly exercise with CoQ10 led to 80% symptom resolution-far better than either alone. Movement helps restore calcium control in muscle cells, even while taking statins.
Switching statins can work. Not all statins are equal. Rosuvastatin and pravastatin are less likely to cause muscle issues than simvastatin or atorvastatin. Lowering the dose also helps-65% of patients tolerate half-dose regimens without losing cholesterol control.
If those don’t work, non-statin options exist:
- Ezetimibe reduces LDL by 15-20% with minimal muscle side effects.
- PCSK9 inhibitors (like evolocumab) lower LDL by 50-60% and have only a 3.7% muscle-related adverse event rate-lower than placebo in some trials.
- Bempedoic acid is a newer oral option that works in the liver, not muscles, and has a very low risk of myopathy.
For the rare autoimmune form (anti-HMGCR myositis), treatment is different. It requires immunosuppression. About 68% of patients go into remission with prednisone and methotrexate within six months.
The Bigger Picture: Why This Matters
Statins are the most prescribed drugs in the U.S., with 39 million users in 2023. Yet adherence drops from 85% to 65% within a year-mostly because of muscle symptoms. That’s not just a personal problem. It’s a public health issue. Patients who stop statins without alternatives have a 25% higher risk of heart attack or stroke over five years.
Pharmaceutical companies are responding. Two new statin candidates-STT-101 and STT-202-are in early trials. They’re designed to stay in the liver and avoid muscle tissue entirely, reducing skeletal muscle concentrations by 70% compared to traditional statins. If successful, they could change the game.
Meanwhile, a promising drug called S107, which stabilizes the RyR1 channel, reduced muscle symptoms by 52% in a 2023 trial. It’s not yet available, but it points to a future where we don’t have to choose between heart protection and muscle comfort.
What Should You Do Now?
If you’re on a statin and feeling muscle pain:
- Don’t stop cold turkey. Talk to your doctor first.
- Track your symptoms: when they started, what makes them better or worse.
- Ask about a washout period-stop the statin for 4 weeks and see if symptoms improve.
- Request a CK test if pain is severe or persistent.
- Start taking 200 mg of CoQ10 daily. It’s safe and may help.
- Get moving. Aim for 30 minutes of brisk walking, cycling, or swimming five days a week.
- Ask if switching to a different statin or trying ezetimibe or PCSK9 inhibitors makes sense for you.
Remember: statins save lives. But they shouldn’t make you feel worse. With the right approach, you can keep your heart protected without sacrificing your mobility.
Can statin muscle pain go away on its own?
Yes, in most cases. About 80% of people who stop their statin see muscle symptoms resolve within 1 to 4 weeks. The body clears the drug, calcium leaks stop, and muscle cells begin to repair. But if symptoms persist beyond a month, it could be a sign of something more serious-like autoimmune myopathy-requiring medical evaluation.
Is CoQ10 really effective for statin muscle pain?
Evidence suggests it helps, but not for everyone. In randomized trials, 200 mg of CoQ10 daily reduced muscle pain in about 35% of patients. It’s most effective when combined with moderate exercise. While it won’t fix autoimmune myopathy or severe cases, it’s a low-risk, well-tolerated option worth trying before switching medications.
Does exercise make statin myopathy worse?
No-it helps. Contrary to old beliefs, moderate exercise doesn’t worsen statin-induced muscle damage. In fact, a 2023 JUPITER trial subanalysis showed exercisers had 32% lower creatine kinase levels and 41% fewer symptoms than sedentary users. Movement appears to stabilize the calcium channels in muscle cells, reducing the leak that causes pain. Aim for 150 minutes of moderate activity per week.
Are some statins less likely to cause muscle pain?
Yes. Pravastatin and rosuvastatin have lower rates of muscle side effects than simvastatin or atorvastatin. This is because they’re less likely to penetrate muscle tissue. If you’re experiencing symptoms, switching to one of these alternatives-or lowering your dose-can often resolve the issue while still controlling cholesterol.
What’s the difference between statin myopathy and rhabdomyolysis?
Statin myopathy refers to muscle pain and weakness with or without elevated creatine kinase. Rhabdomyolysis is a rare, life-threatening form where muscle breaks down rapidly, releasing toxins into the blood that can damage kidneys. It occurs in fewer than 0.1% of statin users and usually involves very high CK levels (over 10,000 U/L), dark urine, and severe weakness. If you have these symptoms, seek emergency care immediately.
Can I take statins again after stopping due to muscle pain?
Many people can. About 40% of patients who switch to a different statin tolerate it well. Another 65% can manage a lower dose. Success is higher if you combine the switch with CoQ10 and regular exercise. Rechallenge should be done under medical supervision, with symptoms monitored closely.
Is statin-induced autoimmune myopathy common?
No-it’s rare, affecting only about 0.02% of statin users. But it’s serious. It usually develops after months or years of use and doesn’t improve after stopping the drug. Blood tests for anti-HMGCR antibodies can confirm it. Treatment requires immunosuppressants like prednisone and methotrexate, and recovery can take months. Early diagnosis is critical.
Why do some doctors still say statins are safe despite muscle pain?
Because for most people, the benefits far outweigh the risks. Statins reduce heart attacks and strokes by 25-30% in high-risk patients. Muscle pain is common but rarely dangerous. The issue is that many patients stop taking statins unnecessarily. Doctors emphasize that muscle symptoms should be managed-not automatically lead to discontinuation. With the right approach, most people can stay on statins safely.


Write a comment