When your nose is constantly stuffed up, your face feels heavy, and your headaches won’t go away-even after taking antihistamines-it might not just be allergies. For millions of people with seasonal or year-round allergies, persistent sinus symptoms are often a sign of sinusitis triggered by allergic inflammation. This isn’t a simple cold that will clear up in a week. It’s a chronic cycle: allergies swell the nasal passages, block sinus drainage, and create the perfect environment for bacteria, fungi, and more inflammation to take hold. Treating it like a regular cold won’t work. You need a targeted approach that tackles both the allergy and the sinus infection together.
Why Allergies Make Sinusitis Worse
Allergic rhinitis and chronic sinusitis are closely linked. Studies show that 65 to 75% of people with chronic sinusitis also have underlying allergies. When you’re exposed to pollen, dust mites, mold, or pet dander, your immune system overreacts. This causes swelling in the nasal lining, which blocks the tiny channels that drain your sinuses. Mucus gets trapped. Bacteria grow. Inflammation sticks around. Over time, this becomes a loop: allergies cause sinusitis, and the inflamed sinuses make your allergies feel even worse.
It’s not just discomfort. People with allergy-related sinusitis have more frequent flare-ups, longer recovery times, and higher chances of developing nasal polyps-soft, noncancerous growths that further block airflow. In fact, up to 30% of chronic sinusitis cases involve nasal polyps, and nearly half of those are tied to allergic triggers. This isn’t something you can ignore. Left untreated, it can lead to ear infections, sleep apnea, or even rare but serious complications like infections spreading to the eyes or brain.
First-Line Treatments That Actually Work
Most people start with over-the-counter antihistamines or decongestants. But here’s the truth: those rarely fix the root problem. For allergy-driven sinusitis, the most effective first step is nasal corticosteroids. These aren’t the same as the steroids athletes abuse. They’re anti-inflammatory sprays that target the nasal lining directly. Options like fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) reduce swelling, open drainage pathways, and decrease mucus production. They take time-usually 2 to 4 weeks of daily use before you feel real relief-but they work better than any oral allergy pill.
Another essential tool is saline nasal irrigation. Using a neti pot or squeeze bottle with distilled or boiled water mixed with a sterile saline packet helps flush out allergens, mucus, and irritants. Do it once or twice a day. It’s cheap, safe, and backed by decades of clinical evidence. But get the water right: using tap water has caused rare but deadly brain infections from a water-borne amoeba called Naegleria fowleri. Always use distilled, sterile, or previously boiled (and cooled) water.
Antibiotics? Only if there’s clear evidence of a bacterial infection-like thick yellow-green mucus, fever, or symptoms lasting more than 10 days. Even then, antibiotics only help about 35-45% of allergy-related cases, compared to 80% in pure bacterial sinusitis. Overusing them leads to resistance and doesn’t fix the allergic trigger.
When Medications Aren’t Enough
If you’ve tried nasal sprays and saline for 4 to 6 weeks and still feel blocked, tired, and congested, it’s time to consider stronger options. For people with nasal polyps or recurrent infections, biologic therapies are changing the game. Drugs like dupilumab (Dupixent) and omalizumab (Xolair) target specific parts of the immune system that drive allergic inflammation. In clinical trials, dupilumab reduced nasal polyp size by 73% and improved breathing in over 70% of users. But they’re expensive-around $3,500 a month without insurance-and require regular injections every 2 to 4 weeks.
A more long-term solution is allergy immunotherapy, commonly called allergy shots. This isn’t a quick fix. It takes 3 to 5 years. You start with weekly injections containing tiny amounts of your allergens, slowly building up your tolerance. By the end, 60 to 70% of patients see a major drop in sinus flare-ups. It’s one of the few treatments that can actually change how your immune system responds to allergens long-term. For people who hate daily sprays or can’t afford biologics, it’s a powerful alternative.
When to See an Ear, Nose, and Throat Specialist
You don’t need to suffer through another winter with constant congestion. If you’ve tried the basics and still struggle, it’s time to see an ENT. Here’s when to refer:
- You’ve used nasal steroids and saline daily for 4 to 6 weeks with no improvement
- You have visible nasal polyps (seen during a nasal exam)
- You get sinus infections 4 or more times a year
- You have symptoms that spread beyond your sinuses-eye swelling, vision changes, severe headaches, or fever
- You suspect aspirin-exacerbated respiratory disease (AERD), which causes severe sinusitis, asthma, and nasal polyps in about 10-15% of chronic cases
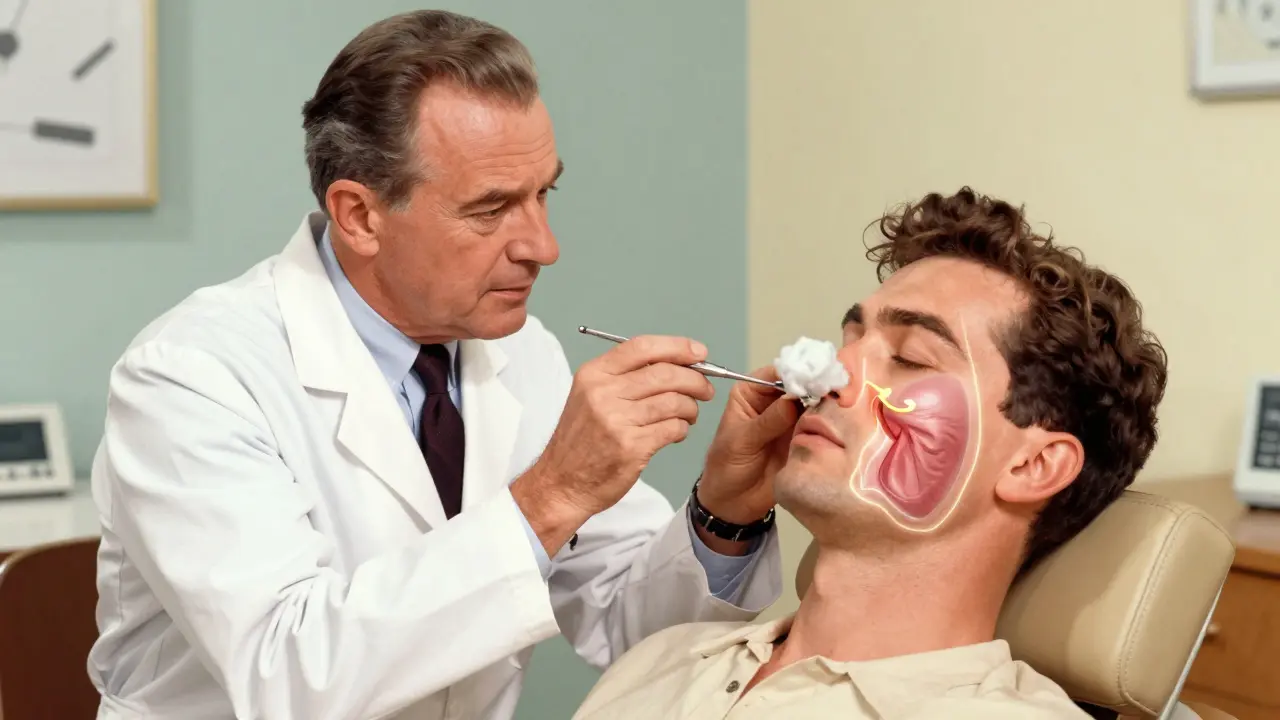
An ENT specialist will likely perform a nasal endoscopy, inserting a thin camera into your nose to look directly at your sinuses. They’ll check for polyps, pus, swelling, or structural issues like a deviated septum. They may also order a CT scan to see the full extent of inflammation. This isn’t just for diagnosis-it helps determine if surgery might be needed.
What Surgery Can and Can’t Do
If medications fail, endoscopic sinus surgery is often the next step. It’s minimally invasive: the surgeon uses tiny instruments and a camera to open blocked sinus passages and remove polyps. Success rates are high-about 85% of patients report better breathing and fewer infections after surgery. But here’s the catch: if you still have uncontrolled allergies, the inflammation comes back. Studies show that 20 to 30% of allergy sufferers develop new polyps or blockages within 5 years after surgery. That’s why surgery alone isn’t a cure. It’s a reset button. You still need to manage your allergies afterward-through sprays, immunotherapy, or environmental control.

Environmental Control: The Hidden Key
One of the most overlooked parts of treatment is reducing your exposure to allergens. Dr. David Stukus, a leading allergist, says environmental control can reduce sinus flare-ups by 40 to 60%. Simple steps make a big difference:
- Use HEPA filters in your bedroom and vacuum cleaner
- Wash bedding weekly in hot water to kill dust mites
- Keep windows closed during high pollen seasons
- Use a dehumidifier if you live in a damp climate-mold thrives in humidity
- Consider removing carpeting, especially in bedrooms
If you live in an urban area, air pollution can make things worse. Studies show city dwellers have 20 to 25% higher rates of chronic sinusitis than people in rural areas. If you’re in Vancouver or another city with high smog levels, consider an air purifier with a carbon filter to trap pollutants.
New Treatments on the Horizon
The field is moving fast. In 2023, the FDA approved tezepelumab (Tezspire) for severe sinusitis with nasal polyps. Early data shows a 56% drop in flare-ups. Researchers are also exploring microbiome therapies-using beneficial bacteria to crowd out harmful ones in the sinuses. Early trials suggest this could reduce antibiotic-resistant infections by nearly half within five years. And in mold-prone areas, doctors are now using intranasal antifungals for select patients, with one trial showing a 32% improvement in symptoms.
Still, access remains unequal. Rural patients wait 30 to 40% longer than urban patients to see a specialist. Biologics are out of reach for many without good insurance. That’s why the most important step isn’t always the most expensive one-it’s recognizing when your current treatment isn’t working and asking for help before things get worse.
What You Can Do Today
If you’ve been living with constant congestion, pressure, and fatigue-and you know you have allergies-it’s time to stop treating it like a nuisance. Start with the basics: use a nasal corticosteroid every day for at least a month. Add saline irrigation twice a day. Track your symptoms. If there’s no change, talk to your doctor about allergy testing. If you have polyps or frequent infections, ask for a referral to an ENT. Don’t wait until you’re on antibiotics every other month. The goal isn’t just to feel better for a few days-it’s to break the cycle for good.
Can allergies cause chronic sinusitis?
Yes. Allergies are one of the leading causes of chronic sinusitis. When allergens like pollen, dust, or mold trigger an immune response, they cause swelling in the nasal passages. This blocks sinus drainage, leading to trapped mucus, bacterial growth, and long-term inflammation. Up to 75% of people with chronic sinusitis have underlying allergies.
Are nasal corticosteroids safe for long-term use?
Yes. Unlike oral steroids, nasal corticosteroids are designed to act locally with minimal absorption into the bloodstream. Studies show they’re safe for daily use over years. Side effects are rare and mild-like nose dryness or occasional bleeding. They’re far safer than long-term antibiotic use or repeated sinus infections.
Do I need antibiotics for sinusitis if I have allergies?
Not usually. Most sinusitis in allergy sufferers is caused by inflammation, not bacteria. Antibiotics only help if symptoms last more than 10 days, get worse after improving, or include high fever and thick pus. Overuse leads to resistance. Focus first on reducing inflammation with nasal sprays and saline irrigation.
How long does allergy immunotherapy take to work?
It takes time. The buildup phase-where doses increase weekly-lasts 4 to 6 months. Then you move to maintenance shots every 2 to 4 weeks for 3 to 5 years. Most people notice fewer sinus infections after 6 to 12 months, but the real benefit comes after 3 years, when your immune system becomes less reactive to allergens.
Can surgery cure sinusitis caused by allergies?
Surgery can open blocked sinuses and remove polyps, improving breathing and reducing infections in about 85% of cases. But if your allergies aren’t controlled afterward, inflammation returns. Surgery is a tool to reset your sinuses-not a cure. You still need ongoing allergy management to prevent recurrence.
What’s the difference between a regular sinus infection and allergy-related sinusitis?
A regular sinus infection often starts with a cold and clears up in 7 to 10 days with or without antibiotics. Allergy-related sinusitis is persistent. It flares up repeatedly, often without a cold, and doesn’t improve with antibiotics alone. Symptoms include ongoing nasal congestion, post-nasal drip, facial pressure, and fatigue that lasts weeks or months. The trigger is allergic inflammation, not just bacteria.


Write a comment