When a patient has a serious reaction to a generic drug, who do you report it to? And more importantly-do you even know how?
The truth is, reporting serious adverse events (SAEs) for generic drugs isn’t just paperwork. It’s a critical part of keeping millions of people safe. Every year, over 90% of prescriptions in the U.S. are filled with generic drugs. But when something goes wrong, those reports rarely make it into the system. And that’s not because the rules are different-it’s because the system is broken.
What Counts as a Serious Adverse Event?
A serious adverse event isn’t just a rash or a headache. The FDA defines it as any reaction that’s life-threatening, causes hospitalization, leads to permanent disability, results in congenital anomalies, or requires medical intervention to prevent lasting harm. This includes heart attacks, liver failure, severe allergic reactions, or sudden loss of consciousness after taking a generic version of a drug like levothyroxine, metoprolol, or simvastatin.
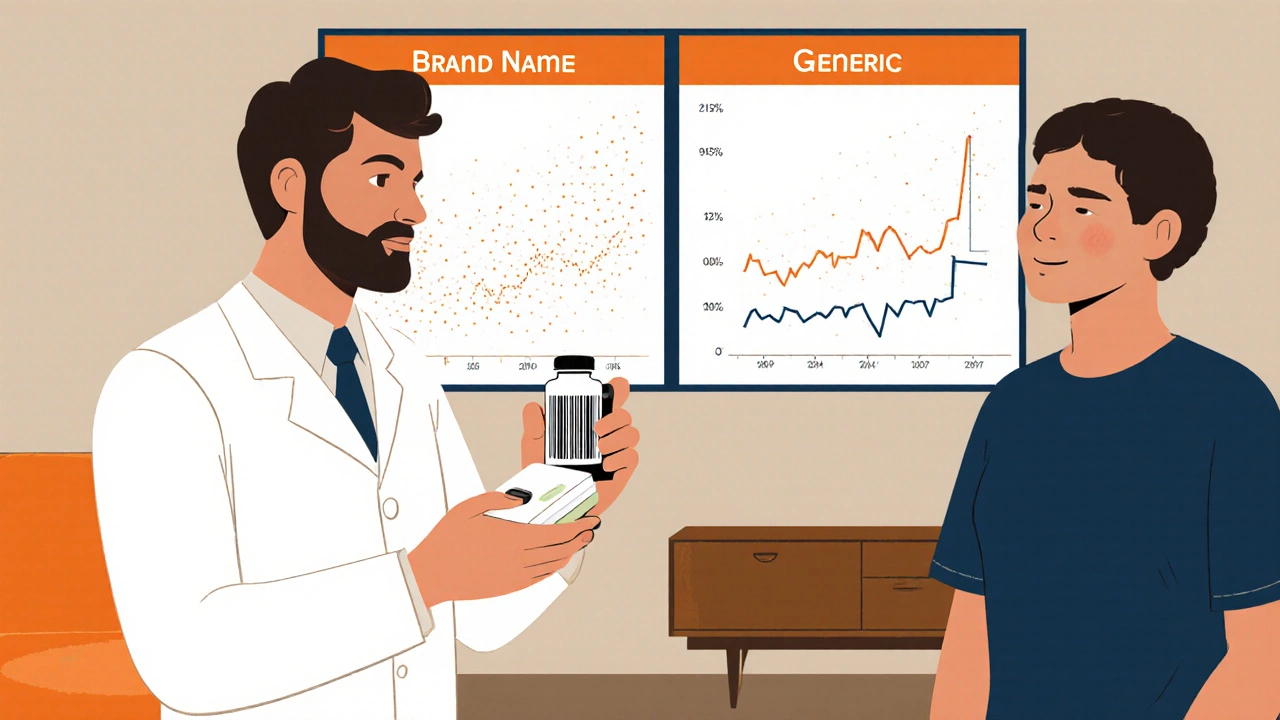
It doesn’t matter if the drug is brand-name or generic. The legal requirement is identical. Under 21 CFR 312.64(b), any healthcare provider or manufacturer who becomes aware of a serious, unexpected reaction must report it. But here’s where things get messy: while brand-name companies submit about 68% of all serious event reports, they only make up about 1% of prescriptions. Generic drugs, which fill nearly all the rest, account for a tiny fraction of those reports.
Who Is Responsible for Reporting?
There are two main players: manufacturers and healthcare providers.
Generic drug manufacturers are legally required to report serious and unexpected adverse events to the FDA within 15 days of learning about them. They must keep records for 10 years. The European Medicines Agency has even tighter deadlines-7 days for fatal or life-threatening events. But here’s the catch: many generic manufacturers are small companies with no dedicated safety team. Some outsource reporting to third parties. Others don’t have the staff to track reactions properly. According to a 2022 industry survey, only 42% of generic manufacturers have a full pharmacovigilance department. Compare that to 98% of brand-name companies.
Healthcare providers-doctors, nurses, pharmacists-are also supposed to report. But many don’t know how. Or worse, they give up because the process is confusing.
The Reporting Process: MedWatch and the Hidden Roadblocks
The FDA’s MedWatch system is the official channel. You can file online, by phone, or by mail using Form 3500. But filling it out for a generic drug isn’t straightforward.
Here’s what you need:
- The active ingredient (e.g., amlodipine, not Norvasc)
- The manufacturer name (e.g., Teva, Mylan, Amneal)
- The National Drug Code (NDC)-a unique 11-digit number on the bottle
- Details of the reaction: when it started, symptoms, outcome
But here’s the problem: patients rarely know which company made their pill. Pharmacies switch suppliers weekly. A patient might get a bottle from Teva one month and Amneal the next. The label doesn’t always make it obvious. A 2020 ISMP survey found that 68% of healthcare providers couldn’t identify the manufacturer when reporting a reaction to a generic drug. That’s why so many reports get filed under the brand name-even when the patient was taking the generic.
And it gets worse. A 2019 FDA study showed that 42% of healthcare workers abandoned their reports for generics because they couldn’t figure out the manufacturer. For brand-name drugs? Only 9% gave up.
Each report takes 15 to 30 minutes for a brand drug. For generics? Often over 45 minutes. You have to dig through the bottle, look up the NDC on DailyMed, cross-reference it with the manufacturer, and hope you got it right. It’s exhausting. And if you mess up, the data is useless.
Why This Gap Matters
This isn’t just about paperwork. It’s about safety.
Generic drugs are chemically identical to their brand-name counterparts. But they’re not always the same. Differences in fillers, coatings, or manufacturing processes can affect how a drug is absorbed. A 2017 JAMA Internal Medicine study by Dr. Jerry Avorn warned that these subtle differences could be going unnoticed because we’re not collecting the right data.
Take levothyroxine. Thousands of patients rely on it for thyroid function. Even small changes in absorption can cause fatigue, weight gain, or heart palpitations. But if every reaction gets reported as “brand-name levothyroxine,” we’ll never know if one generic manufacturer’s version is causing more issues than others.
The FDA’s own 2018 Drug Safety Newsletter admitted: “We recognize potential limitations in the current system as it relates to generic drugs.” A 2021 Government Accountability Office report confirmed: “FDA lacks sufficient data to determine if adverse events for generics are underreported.” That’s not just a gap-it’s a blind spot.
What’s Being Done to Fix It?
Change is coming-but slowly.
In 2023, the FDA launched FAERS 2.0, a new system that links adverse events directly to NDC codes. That means even if you don’t know the manufacturer’s name, the system can still trace the drug back to the source. It’s a big step.
The FDA also released draft guidance in June 2023 asking pharmacies to print the manufacturer name on every prescription label. Right now, it’s often in tiny font on the side. If it’s front and center, patients and providers can report accurately.
Some hospitals are already ahead of the curve. A pilot program at 12 hospital systems used barcode scanners at the point of administration. When a nurse scans the pill bottle, the system automatically logs the manufacturer and NDC. Result? Generic adverse event reporting jumped by 63%.
The Generic Drug User Fee Amendments (GDUFA III), running from 2023 to 2027, is allocating $15 million specifically to improve generic drug safety monitoring. And generic manufacturers? They’re starting to invest. Spending on pharmacovigilance tools is projected to grow from $185 million in 2023 to $320 million by 2027.

What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s how to report correctly:
- Check the pill bottle. Look for the manufacturer name and NDC number. It’s usually on the side or bottom.
- Use DailyMed. Go to dailymed.nlm.nih.gov and enter the NDC to find the manufacturer.
- Report using MedWatch. Go to fda.gov/medwatch and select “Generic Drug” under product type. Fill in the active ingredient and manufacturer name.
- Document everything. Note the date the reaction started, what symptoms appeared, and what happened afterward.
- Encourage patients. Tell them to keep their pill bottles until the prescription is done. That’s their best tool for accurate reporting.
If you’re a pharmacist, advocate for barcode scanning at your pharmacy. If you’re a doctor, ask your pharmacy to include manufacturer info on labels. If you’re a patient, don’t toss that bottle. It might save someone’s life.
The Bigger Picture
Generic drugs save the U.S. healthcare system over $300 billion a year. They’re essential. But safety can’t be an afterthought. If we keep pretending all generics are the same, we risk missing real dangers.
Reporting isn’t just a formality. It’s the only way we find out when something isn’t working. Every report matters-even if it’s just one patient, one bottle, one manufacturer. Without accurate data, regulators can’t act. Patients stay at risk. And the system stays broken.
It’s time to treat generic drug safety like it’s just as important as brand-name safety. Because it is.
Do I have to report a serious adverse event if I’m not the manufacturer?
Yes. Healthcare providers-including doctors, nurses, and pharmacists-are legally encouraged to report serious adverse events to the FDA through MedWatch, even if they’re not the drug manufacturer. The FDA relies on frontline providers to catch reactions that manufacturers might miss. Reporting is voluntary for providers but strongly recommended as part of patient safety.
What if I don’t know which generic manufacturer made the drug?
If you don’t know the manufacturer, check the pill bottle for the National Drug Code (NDC) number. You can enter that number into the DailyMed database (dailymed.nlm.nih.gov) to find the manufacturer. If the bottle is gone, report using the active ingredient and note “manufacturer unknown.” The FDA can still track the drug using the NDC if it’s in the patient’s pharmacy records.
Can I report a reaction even if it’s not confirmed to be caused by the drug?
Yes. The FDA only requires reporting of serious and unexpected reactions that may be “reasonably possible” or “probably caused” by the drug. You don’t need proof-just a reasonable suspicion. The system is designed to catch signals early, so even uncertain reports help build the safety picture over time.
How long do I have to report a serious adverse event?
Manufacturers must report serious, unexpected events within 15 calendar days of learning about them. Healthcare providers have no strict deadline, but reports should be submitted as soon as possible. Delayed reports reduce the ability to detect patterns or emerging safety issues. The sooner you report, the better.
Are there penalties for not reporting?
Healthcare providers are not legally penalized for failing to report. But manufacturers who fail to report serious adverse events within the required timeframe can face FDA enforcement actions, including warning letters, fines, or even product recalls. The FDA considers accurate reporting a core part of drug safety compliance.
Why do brand-name drugs get reported more often than generics?
Brand-name companies have large pharmacovigilance teams, dedicated hotlines, and patient support programs that actively collect reports. Generic manufacturers-especially smaller ones-often lack resources. Patients also rarely know which generic company made their pill, so reports get misattributed to the brand name. This creates a reporting gap that’s been documented for over a decade.
Can I report an adverse event for a generic drug that’s not on the FDA’s list?
Yes. The FDA accepts reports for any drug marketed in the U.S., including generics that are approved under an Abbreviated New Drug Application (ANDA). Even if the drug isn’t listed in public databases yet, if it’s legally available and you observe a serious reaction, report it. The FDA uses all reports to monitor safety, regardless of how new or obscure the product is.
Next Steps: What to Do After Reporting
After you submit a report, the FDA logs it into the FAERS database. It’s anonymous and aggregated. No single report will trigger an immediate action-but thousands of similar reports can. That’s how safety signals are found.
If you’re a provider, follow up with your pharmacy. Ask if they can label generic bottles with the manufacturer name. If you’re part of a clinic or hospital, push for barcode scanning at the point of dispensing. It’s one of the most effective ways to close the reporting gap.
And if you’re a patient? Keep your pill bottles. Don’t throw them out until the prescription is done. That small habit could make all the difference when it comes time to report-or help someone else avoid a reaction.
Generic drugs are the backbone of affordable care. But safety doesn’t come cheap. It comes from attention, accuracy, and action. Don’t assume someone else is reporting. Do it yourself. Because when it comes to drug safety, no report is too small.

Write a comment