Quercetin Medication Interaction Checker
Check for Quercetin Interactions
Enter your prescription medications below to see if quercetin supplements could cause dangerous interactions. Quercetin can significantly increase drug levels for many medications, especially at doses above 500 mg per day.
Interaction Analysis Results
Based on the latest research about quercetin interactions with medications
Remember: Quercetin from food (apples, onions, berries) is safe. The danger comes from supplements containing high doses (500mg+ per day).
Most people think of quercetin as just another natural antioxidant found in apples, onions, and berries. It’s marketed as a supplement for inflammation, allergies, or immune support. But if you’re taking any prescription meds, especially heart drugs, blood thinners, or cancer treatments, quercetin could be quietly changing how your body handles those drugs - and not in a good way.
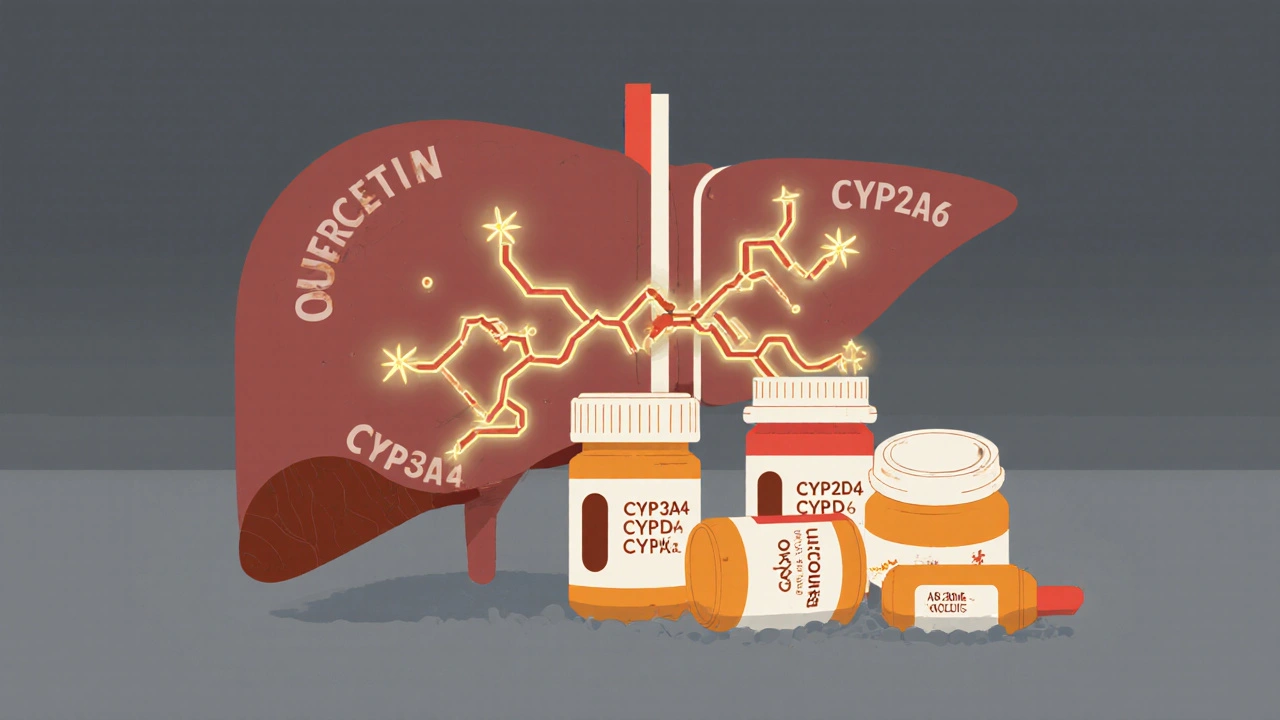
What Quercetin Actually Does Inside Your Body
Quercetin isn’t just a plant compound. When taken as a supplement - especially in doses over 500 mg per day - it acts like a molecular wrench thrown into your body’s drug-processing system. Your liver and intestines use enzymes called cytochrome P450 (CYP) to break down most medications. Quercetin shuts down key ones: CYP3A4, CYP2D6, and CYP2C19. These aren’t minor players. Together, they handle more than 70% of all prescription drugs.
Think of it like traffic control. Normally, your body slows down and clears out drugs at a steady pace. Quercetin slams the brakes. That means drugs like abemaciclib (a cancer drug), cyclosporine (a transplant medication), or even common painkillers like acetaminophen stick around longer. Blood levels can jump by 20% to over 300%, depending on the drug and dose. In one study, people taking quercetin supplements saw midazolam (a sedative) levels rise 2.3 times higher than normal.
It’s Not Just About Liver Enzymes
Quercetin doesn’t stop at enzymes. It also blocks transporters - the proteins that move drugs into and out of cells. Two major ones affected are OATP1B1 and BCRP. These are the gates that let drugs like statins, blood thinners, and chemotherapy agents enter the liver or exit the gut. When quercetin clogs them, drugs pile up in your bloodstream instead of being properly absorbed or cleared.
For example, apixaban and rivaroxaban - direct oral anticoagulants used to prevent strokes - are moved by these transporters. When quercetin blocks them, drug levels rise 20-35%. That’s not a small risk. It means you could bleed internally without warning. The American Society of Health-System Pharmacists warns: avoid quercetin entirely if you’re on these drugs.
Who’s at the Highest Risk?
Not everyone who takes quercetin will have a problem. But certain people are sitting on a time bomb:
- People over 65 - older adults clear quercetin 25-40% slower, so it builds up faster.
- Those on narrow therapeutic index drugs - where the difference between a helpful dose and a toxic one is tiny. Think warfarin, cyclosporine, digoxin, or certain seizure meds.
- People taking multiple medications - the more drugs you take, the more chances quercetin will interfere with one of them.
- Those taking high-dose supplements - 500 mg or more per day. That’s far beyond what you get from food.
Here’s the scary part: in 2021, nearly 1 in 5 Americans using quercetin supplements were taking over 500 mg daily. And 23% were taking more than 1,000 mg - the exact dose the European Food Safety Authority flagged as risky for drug interactions.

What Drugs Are Most Affected?
Quercetin doesn’t play favorites. It hits a wide range. Here are the top categories and examples:
- Blood thinners: Warfarin (INR can spike by 0.8-1.5 points), apixaban, rivaroxaban
- Immunosuppressants: Cyclosporine, tacrolimus - levels can rise 30-50%, risking kidney damage
- Cancer drugs: Abemaciclib, dasatinib - higher levels mean more side effects like low blood counts
- Heart meds: Diltiazem, verapamil, amiodarone - increased risk of low blood pressure or irregular heartbeat
- Antidepressants and anti-anxiety drugs: Sertraline, fluoxetine, buspirone - metabolized by CYP2D6, which quercetin strongly blocks
- Pain relievers: Acetaminophen - levels rise 20-30%, raising liver toxicity risk
Even something as simple as ibuprofen or omeprazole can be affected. And here’s the twist: if you take quercetin in food - say, an apple or red onion - you’re fine. The amount is too low. But supplements? That’s a different story. A single capsule can deliver 500 mg. That’s 100 times more than you’d get from eating a cup of capers.
Why Food Is Safe, But Supplements Aren’t
Quercetin in food comes bound to sugars (called glycosides), like rutin. Your body breaks these down slowly, so levels stay low and steady. But supplements use the pure, unbound form - called the aglycone. That’s the form that’s a powerful enzyme blocker. One study found glycosides like rutin are 60-70% less potent than pure quercetin. So eating onions won’t hurt you. Taking a quercetin pill? That’s where the danger starts.
What the Experts Are Saying
The FDA calls quercetin a "dietary supplement of concern" for drug interactions. The European Medicines Agency says the lab data is clear, but human evidence is still limited - mostly because people don’t report these interactions. Underreporting is estimated at 90-95%. That means for every reported case, there are 20 more going unnoticed.
Pharmacists at UCSF and other major hospitals now have protocols: if a patient is on a CYP3A4, CYP2D6, or CYP2C19 substrate, they’re told to avoid quercetin supplements above 500 mg/day. For elderly patients or those on multiple meds? Avoid it entirely.
And it’s not just doctors. The supplement industry is growing fast - $387 million in sales in 2022. But regulation? Barely any. Under U.S. law (DSHEA), manufacturers don’t need to prove safety before selling. The FDA has issued 17 warning letters to quercetin brands since 2018 for making false claims - but no recalls. No mandatory labeling. No warning labels about drug interactions.
What Should You Do?
If you’re taking any prescription medication and use quercetin supplements, here’s your action plan:
- Stop taking quercetin supplements if you’re on blood thinners, immunosuppressants, cancer drugs, or heart meds.
- Check your labels. Many supplements list "quercetin" under "antioxidant blend" or "immune support formula." Look for the amount per serving.
- Talk to your pharmacist. They have access to drug interaction databases. Bring your full supplement list - not just the big names.
- If you must take it, separate it from your meds by 4-6 hours. That can reduce interaction risk by 30-50%.
- Don’t assume "natural" means safe. Quercetin is a powerful bioactive compound. It’s not harmless just because it comes from a plant.
There’s no reason to panic if you eat a salad with onions and apples. But if you’re popping pills labeled "quercetin 500 mg" because you read it "boosts immunity," you’re playing Russian roulette with your meds. The science is clear. The risks are real. And no one’s warning you.
What’s Coming Next?
The FDA is working on a 2024 rule that would require supplement makers to label potential drug interactions - especially for high-risk compounds like quercetin. Clinical trials are underway to pin down exact interaction levels. But until then, you’re on your own.
The bottom line: if you’re on medication, treat quercetin supplements like you would a new prescription. Ask your doctor. Check with your pharmacist. Don’t guess. Because when it comes to drug interactions, the quiet ones are the deadliest.
Can I take quercetin if I’m on blood thinners like warfarin?
No. Quercetin can increase warfarin levels by 30-45%, raising your INR by 0.8 to 1.5 points. That significantly increases your risk of serious bleeding, including internal bleeding or stroke. Even small changes in INR can be dangerous. Avoid quercetin supplements entirely if you’re on warfarin or any other blood thinner.
Does quercetin interact with statins like atorvastatin?
Yes. Atorvastatin is metabolized by CYP3A4, which quercetin strongly inhibits. This can raise atorvastatin levels by 20-50%, increasing the risk of muscle damage (rhabdomyolysis), liver toxicity, and kidney problems. If you take statins, avoid quercetin supplements. Eating onions or apples is fine - the dose is too low to matter.
How much quercetin is too much to cause interactions?
Doses above 500 mg per day pose a real risk for drug interactions. The European Food Safety Authority specifically flagged doses over 1,000 mg/day as concerning. Most supplement capsules contain 500-1,000 mg. The amount you get from food - even a whole day’s worth - is less than 10 mg. So the danger comes from supplements, not diet.
Is quercetin from onions and apples safe with medications?
Yes. Quercetin in food is bound to sugars (like rutin), which your body absorbs slowly and converts into less active forms. You’d need to eat over 10 pounds of onions daily to reach the 500 mg dose linked to drug interactions. So eating a normal diet with fruits and vegetables is safe - even if you’re on medication.
Can I just take quercetin a few hours after my meds to avoid interactions?
Spacing them out by 4-6 hours can reduce interaction risk by 30-50%, based on pharmacokinetic modeling. But it’s not a guarantee. For high-risk drugs like cyclosporine, abemaciclib, or DOACs, avoidance is still the safest option. If you’re unsure, talk to your pharmacist. Don’t rely on timing alone.
Why don’t supplement labels warn about drug interactions?
Under U.S. law (DSHEA), supplement makers don’t have to prove safety or efficacy before selling. They also don’t have to list drug interaction warnings. The FDA has issued 17 warning letters to quercetin brands for making false claims, but no labeling rules exist yet. A proposed 2024 rule may change that, but until then, you have to do your own research.
Are there any supplements that are safer alternatives to quercetin?
If you’re looking for anti-inflammatory or antioxidant support without interaction risks, consider vitamin C, vitamin D, or omega-3s - all have strong safety profiles with medications. Curcumin (from turmeric) has some interaction potential too, but it’s generally lower than quercetin. Always check with your pharmacist before starting any new supplement, even if it’s "natural."

Write a comment