When you’re taking more than one psychiatric medication, it’s not just about whether each drug works on its own-it’s about what happens when they meet inside your body. Some combinations can be safe and even helpful. Others? They can land you in the emergency room. This isn’t theory. It’s happening right now, in clinics and homes across the country, often because no one checked the interactions.
Why Some Mixes Are Deadly
The biggest danger comes from drugs that boost serotonin too much. Serotonin is a chemical your brain uses to regulate mood, sleep, and even digestion. Too little, and you feel low. Too much, and you get serotonin syndrome-a potentially fatal condition. Symptoms start with shivering, diarrhea, and confusion, then quickly turn to high fever, seizures, irregular heartbeat, and loss of consciousness. The most dangerous combo? Taking an MAO inhibitor like phenelzine (Nardil) with any SSRI or SNRI. This isn’t a rare mistake. It’s one of the most common causes of preventable psychiatric deaths. MAO inhibitors block the breakdown of serotonin. SSRIs like fluoxetine or sertraline flood your system with more of it. Together? Your serotonin levels can skyrocket in hours. The risk is so high that doctors require a 14-day washout period between stopping an MAOI and starting an SSRI. No exceptions.SSRIs and SNRIs: The Most Common Culprits
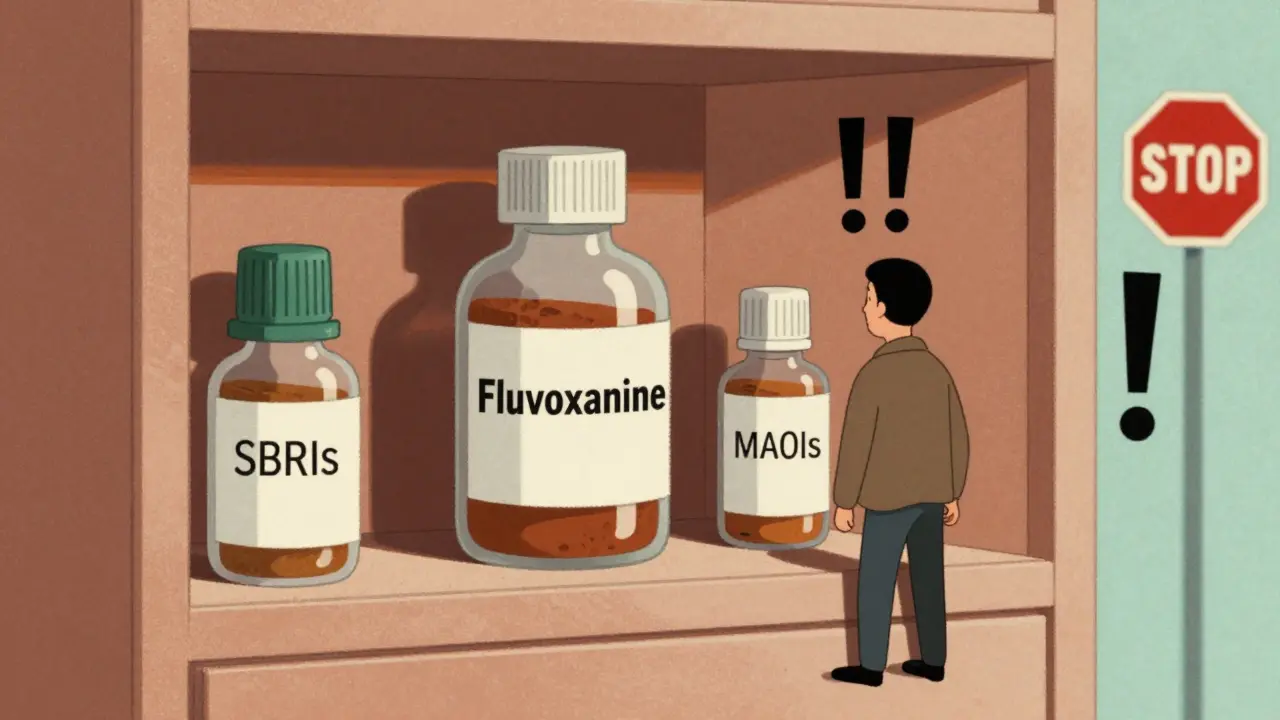
SSRIs (selective serotonin reuptake inhibitors) and SNRIs (serotonin-norepinephrine reuptake inhibitors) are the most prescribed psychiatric meds in North America. Fluoxetine, sertraline, escitalopram, venlafaxine-they’re everywhere. But not all are created equal when it comes to interactions. Fluvoxamine is the worst offender. It shuts down three key liver enzymes-CYP1A2, CYP2C19, and CYP3A4-that break down dozens of other drugs. If you’re on fluvoxamine and take clozapine, the antipsychotic, your clozapine levels can jump by 300%. That’s not a tweak. That’s overdose territory. Even common OTC meds like dextromethorphan (in cough syrups) can trigger serotonin syndrome when mixed with fluvoxamine. Sertraline and citalopram? Much safer. They barely touch those liver enzymes. That’s why many psychiatrists pick them first when someone’s already on other meds. If you’re on warfarin, a blood thinner, sertraline is a better choice than fluoxetine. Warfarin levels can spike 20-30% with fluoxetine, raising your risk of internal bleeding. With sertraline? The change is negligible.TCAs and the Silent Cardiovascular Threat
Tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline are older, but still used-especially for chronic pain or severe depression. They’re powerful, but they’re also toxic if combined wrong. TCAs block acetylcholine, which causes dry mouth, constipation, and blurred vision. But they also mess with your heart rhythm. When paired with antipsychotics like haloperidol or even some antihistamines like diphenhydramine (Benadryl), they can cause QT prolongation-a dangerous heart rhythm issue that can lead to sudden cardiac arrest. Add alcohol to the mix? Sedation multiplies. Coordination vanishes. Falls and accidents become likely. And don’t forget lithium. Many people take lithium for bipolar disorder. It has a tiny window between working and poisoning. Normal levels: 0.6-1.0 mmol/L. Over 1.2? You’re in danger. NSAIDs like ibuprofen or naproxen reduce kidney clearance of lithium. One study showed lithium levels rising 25-50% after just a few days of NSAID use. That’s why patients on lithium are told to avoid these painkillers. If you need pain relief, acetaminophen is the only safe option.Antipsychotics: Not All the Same
Antipsychotics like risperidone, quetiapine, and olanzapine are often added to antidepressants for treatment-resistant depression or bipolar disorder. But their interaction profiles vary wildly. Quetiapine? Low risk. It doesn’t strongly inhibit liver enzymes. You can usually mix it with SSRIs without major concern. But fluvoxamine? That’s a different story. Fluvoxamine is an SSRI, but it’s also a powerful CYP enzyme blocker. When combined with olanzapine or risperidone, levels of those antipsychotics can climb dangerously high. Patients end up with extreme drowsiness, low blood pressure, or even delirium. Clozapine is the most dangerous of all. It can cause agranulocytosis-a drop in white blood cells that leaves you defenseless against infections. It requires weekly blood tests for the first six months. If you’re on clozapine and start fluvoxamine? Your clozapine levels can double. That’s why you never start fluvoxamine without consulting your psychiatrist first.MAO Inhibitors: The One You Can’t Afford to Mess Up
MAO inhibitors like phenelzine and tranylcypromine are rarely used today. But when they are, they demand extreme caution. These drugs stop your body from breaking down tyramine-a compound found in aged cheeses, cured meats, soy sauce, and tap beer. Eat one of these while on an MAOI, and your blood pressure can spike to stroke-levels in minutes. But the real killer? Combining MAOIs with serotonergic drugs. Even a single dose of tramadol, an opioid painkiller, can trigger serotonin syndrome in someone on an MAOI. The same goes for dextromethorphan, St. John’s wort, or even certain migraine meds like sumatriptan. There’s no gray area here. If you’re on an MAOI, you must avoid all SSRIs, SNRIs, tramadol, dextromethorphan, and St. John’s wort. Period. No exceptions. No "just one pill." The risk isn’t theoretical. It’s deadly.
What You Can Do to Stay Safe
You don’t need to be a doctor to protect yourself. Here’s what works:- Keep a full list of every pill, supplement, and OTC drug you take-including herbal teas and sleep aids. Bring it to every appointment.
- Ask your pharmacist every time you get a new prescription: "Is this safe with what I’m already taking?" Pharmacists are trained for this. Use them.
- Never start a new med without a plan. If you’re adding an SSRI to an existing antipsychotic, ask: "Will I need monitoring? How often? What symptoms should I watch for?"
- Know your warning signs. Shivering, confusion, fast heartbeat, high fever-these aren’t normal side effects. They’re red flags. Go to the ER if you feel them.
- Use digital tools. Apps like Medscape or Epocrates let you scan your meds and check interactions in seconds. Many clinics now use these systems to flag risks before prescriptions are filled.
When to Call for Help
Most dangerous interactions show up within the first few days of starting a new drug. That’s why the first dose matters. If you’ve just started a new psychiatric med-or added one to your current list-pay attention for the next 72 hours. Watch for:- Unexplained sweating or fever
- Agitation or hallucinations
- Fast heartbeat or dizziness
- Muscle stiffness or tremors
What’s Changing Now
The field is getting smarter. Genetic testing for CYP2D6 and CYP2C19 enzymes is now available in many clinics. These tests tell you if your body breaks down certain drugs slowly-or not at all. If you’re a slow metabolizer, even a normal dose of an SSRI could build up to toxic levels. That’s why some psychiatrists now test before prescribing. Digital tools are also catching on. Hospitals in Vancouver, Toronto, and Seattle are using AI systems that cross-reference your full medication list in real time. One study showed a 37% drop in serious interactions when these systems were used with clinician training. The message is clear: psychiatric polypharmacy isn’t inherently bad. But it’s not harmless, either. The key isn’t avoiding multiple meds-it’s managing them with precision, awareness, and respect for how they interact.Can I take ibuprofen with lithium?
No. Ibuprofen and other NSAIDs can raise lithium levels by 25-50%, pushing you into toxic range. This can cause tremors, confusion, kidney damage, or seizures. Use acetaminophen (Tylenol) instead for pain or fever if you’re on lithium.
Is it safe to mix antidepressants with alcohol?
It’s not recommended. Alcohol can worsen sedation, dizziness, and impaired coordination-especially with TCAs, MAOIs, and some antipsychotics. It can also make depression or anxiety worse over time. Even one drink can increase your risk of falls or accidents.
What’s the safest SSRI to take with other meds?
Sertraline and citalopram have the lowest interaction risk among SSRIs. They don’t strongly block liver enzymes like fluvoxamine does. That’s why they’re often the first choice when someone is already on other medications like antipsychotics or blood thinners.
Can I take St. John’s wort with my antidepressant?
Never. St. John’s wort is a natural supplement that boosts serotonin. When combined with SSRIs, SNRIs, or MAOIs, it can trigger serotonin syndrome-a life-threatening condition. Even if you think it’s "natural," it’s not safe with psychiatric meds.
How long should I wait after stopping an MAOI before starting an SSRI?
At least 14 days. This is non-negotiable. MAOIs stay active in your body for weeks. Starting an SSRI too soon can cause serotonin syndrome. Your doctor should give you a clear washout plan. Don’t skip it.

Write a comment