Itching that won’t quit - no rash, no bug bite, just relentless, deep-seated itchiness that keeps you up at night. For people with cholestatic liver disease, this isn’t just annoying. It’s debilitating. Up to 70% of those with primary biliary cholangitis (PBC) experience it. And it’s not caused by allergies or dry skin. This is cholestatic pruritus, a symptom tied directly to how bile flows - or doesn’t - in the liver.
Why Does Cholestasis Cause Itching?
When bile can’t flow properly - whether due to blocked ducts, autoimmune damage, or pregnancy-related changes - substances build up in the blood. For decades, doctors thought it was just bile acids irritating nerve endings. But research now points to a more complex picture. Lysophosphatidic acid (LPA), triggered by an enzyme called autotaxin, plays a major role. It activates itch-sensing nerves in the skin. Endogenous opioids and serotonin also contribute. The key takeaway? This isn’t histamine-driven. That’s why antihistamines like Benadryl or Zyrtec rarely help - despite how often they’re prescribed.
First-Line Treatment: Bile Acid Resins
Cholestyramine (brand name Questran) is still the go-to starting point. It’s not a drug that enters your bloodstream. Instead, it’s a resin that binds bile acids in your gut, trapping them so they’re flushed out in stool instead of being reabsorbed. That breaks the cycle.
The standard dose starts at 4 grams once a day, slowly increasing to 16-24 grams daily in divided doses. But here’s the catch: it tastes like chalky sand. A 2020 survey in Liver International found 78% of patients hated the texture. Many mix it with apple sauce, juice, or yogurt - but even then, 65% stop using it within three months because of the taste or side effects like bloating, constipation, or nausea.
It works for about half to two-thirds of people who stick with it. But if you don’t see improvement after four weeks, it’s time to move on. Cholestyramine also interferes with other medications. If you take thyroid pills, blood thinners, or birth control, you need to take them at least 4-6 hours before or after cholestyramine. Missing that window can make your other drugs useless.
Second-Line: Rifampin
If cholestyramine fails, rifampin (Rifadin) is next. Originally an antibiotic for tuberculosis, it’s now used off-label for itching. It works by boosting liver enzymes that help clear toxins - including those causing itch. In PBC patients, it reduces itching in 70-75% of cases within four weeks.
The dose is 150-300 mg daily. Side effects? Orange or red urine (harmless, but startling), mild nausea, and occasional liver enzyme spikes. About 15-20% of users see elevated transaminases, so liver tests are monitored closely. It also interacts with dozens of medications by speeding up their metabolism. Birth control, statins, and even some antidepressants can become less effective. Still, for many, the trade-off is worth it. One patient on Reddit wrote: “Rifampin turned my pee orange, but my itching dropped from 8/10 to 3/10 in two weeks. Worth it.”

Third-Line: Naltrexone and Sertraline
When rifampin doesn’t cut it or isn’t tolerated, two other options come into play: naltrexone and sertraline.
Naltrexone blocks opioid receptors in the brain. Since endogenous opioids are involved in cholestatic itch, this helps. Dosing starts low - 6.25 mg daily - and increases weekly to 50 mg. Response rates are 50-65%. But the first few days? Rough. About 30% of patients report opioid withdrawal-like symptoms: nausea, anxiety, sweating, even insomnia - even if they’ve never used opioids. That’s why slow titration is non-negotiable.
Sertraline (Zoloft), an SSRI antidepressant, is used off-label. It’s less effective overall - around 40-50% response - but shines in patients with depression or anxiety alongside their itching. It’s easier to tolerate than naltrexone and doesn’t have the same drug interactions. But it doesn’t help much in non-PBC cholestasis, like PSC or bile duct obstruction.
New Hope: Maralixibat and Beyond
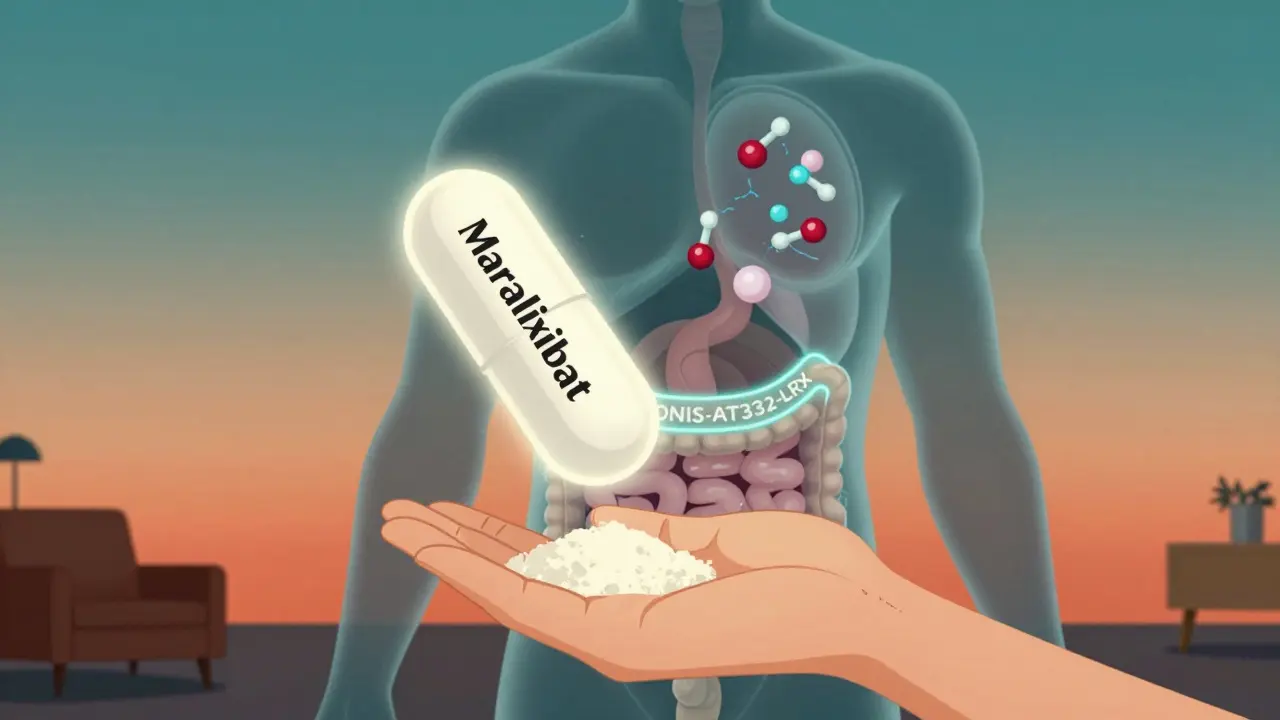
The biggest shift in treatment is happening now. Maralixibat (Mytesi), approved by the FDA in 2021 for Alagille syndrome, is changing the game. It blocks the ileal bile acid transporter (IBAT), stopping bile acids from being reabsorbed in the gut. Unlike cholestyramine, it’s a daily pill with no gritty texture. In trials, it reduced itch by 47% on a 10-point scale - similar to cholestyramine - but with only a 12% discontinuation rate compared to 35% for cholestyramine.
Cleveland Clinic’s 2023 survey found 82% of patients stayed on maralixibat after six months. Why? “No taste issues,” “once-daily dosing,” and “no constipation” were top reasons. The catch? Cost. At $12,500 a month, it’s out of reach for many without insurance. Cholestyramine? About $65 a month.
Other promising drugs are in the pipeline. Volixibat, another IBAT inhibitor, showed 52% itch reduction in a 2023 trial. Then there’s IONIS-AT332-LRx - an antisense drug that knocks down autotaxin production. In a 2023 phase 2 trial, it cut serum autotaxin by 65% and reduced itching by 58%. This could be the first therapy to target the root cause, not just the symptoms.
When All Else Fails: Transplant
For the small number of patients whose itching doesn’t respond to any medication - and who are suffering severely - liver transplant remains the only definitive cure. Studies show 95% of patients experience complete resolution of pruritus after transplant. But it’s a major surgery with lifelong risks. It’s reserved for those with advanced disease, not just itching alone.
What Doesn’t Work - And Why Doctors Still Prescribe It
Despite guidelines from AASLD and EASL clearly stating that antihistamines have no proven benefit in cholestatic pruritus, a 2022 survey found 68% of primary care doctors still prescribe them first. Why? Because itching = allergy in most people’s minds. But cholestatic itch isn’t histamine-related. Giving someone diphenhydramine is like treating a broken leg with a bandage. It might make the patient feel heard, but it doesn’t fix the problem.
Practical Steps for Patients
Here’s what works in real life:
- Start with gentle skin care: Use fragrance-free moisturizers, take cool showers, wear loose cotton clothes.
- Try cholestyramine - but mix it well and give it 4 weeks. If it’s unbearable, talk to your doctor about alternatives.
- If itching persists, ask about rifampin. Get liver tests before and during treatment.
- If rifampin fails or causes side effects, discuss naltrexone or sertraline. Start low, go slow.
- If you have PBC and insurance covers it, ask about maralixibat. It’s expensive, but life-changing for many.
- Never ignore itching. If it’s new or worsening, get checked for biliary obstruction - sometimes a stent can fix it fast.
The Future Is Targeted
Five years ago, treating cholestatic itch meant guessing. Now, we’re targeting specific pathways: bile acid transport, autotaxin, opioid signaling. The goal isn’t just to dull the itch - it’s to stop it at the source. As one hepatologist put it: “We’re moving from treating symptoms to targeting specific pruritogenic pathways.”
That’s huge. For patients who’ve spent years sleeping with ice packs on their arms, or wearing gloves at night to stop scratching, this isn’t just science - it’s relief. And for the first time, there’s real hope that the itch won’t just be managed… it will be silenced.
Is cholestyramine the only first-line treatment for cholestatic pruritus?
No, cholestyramine is the most commonly used first-line option, but it’s not the only one. Lifestyle changes like cool showers, moisturizers, and loose clothing are recommended alongside it. However, if cholestyramine is poorly tolerated or ineffective after four weeks, guidelines recommend moving to second-line therapies like rifampin rather than continuing with higher doses.
Why don’t antihistamines work for cholestatic itching?
Cholestatic pruritus is not caused by histamine release, which is what triggers allergic itching. Instead, it’s driven by bile acids, lysophosphatidic acid (LPA), and endogenous opioids acting on nerve pathways in the skin. Antihistamines block histamine receptors - which aren’t involved here - so they offer little to no relief. Despite this, many doctors still prescribe them due to outdated assumptions about itching.
Can rifampin cause liver damage?
Yes, rifampin can cause elevated liver enzymes in 15-20% of patients, especially with prolonged use. That’s why regular blood tests are required during treatment. While it’s generally safe under monitoring, it should be avoided in patients with pre-existing severe liver dysfunction. The benefits often outweigh the risks in PBC patients with severe itching, but close follow-up is essential.
How does maralixibat compare to cholestyramine?
Maralixibat and cholestyramine both reduce itching by about 40-50% on average, but maralixibat is far better tolerated. Cholestyramine has a 35% discontinuation rate due to taste and GI side effects, while maralixibat’s discontinuation rate is only 12%. Maralixibat is a daily pill with no taste or texture issues, but it costs over $12,000 per month, compared to $65 for cholestyramine. Access remains a major barrier.
Is liver transplant the only cure for cholestatic pruritus?
Liver transplant is the only treatment that reliably cures cholestatic pruritus - with 95% of patients reporting complete resolution after transplant. However, it’s reserved for patients with end-stage liver disease or those whose quality of life is severely impacted despite all other treatments. It’s not recommended solely for itching unless other therapies have failed and liver function is declining.
Are there any new drugs on the horizon for cholestatic pruritus?
Yes. Volixibat, another IBAT inhibitor, showed 52% itch reduction in phase 3 trials. More promising are autotaxin inhibitors like IONIS-AT332-LRx, which target the root cause by reducing LPA production. In a 2023 trial, it cut autotaxin levels by 65% and reduced itching by 58%. These drugs represent the next wave of targeted therapy, moving beyond symptom control to modifying the disease process itself.


Write a comment