It’s 2025, and you’re filling a prescription for generic metformin-a drug that’s been used safely for decades to manage type 2 diabetes. You expect it to be easy. But your pharmacist says, "Your insurance won’t cover it until your doctor gets approval." You’re confused. Why would insurance block a cheap, widely used generic? This isn’t rare anymore. Across the U.S., more than 1 in 5 generic prescriptions now require prior authorization before they’re covered. And it’s making patients wait, doctors frustrated, and healthcare costs go up-not down.
What Is Prior Authorization, Really?
Prior authorization is a gatekeeping step where your insurance company demands proof that a medication is "medically necessary" before they pay for it. For years, this only applied to expensive brand-name drugs or specialty treatments. But now, even simple generics like lisinopril for high blood pressure, levothyroxine for hypothyroidism, or atorvastatin for cholesterol are being caught in the same net.The goal was always to prevent unnecessary spending. But today, it’s doing the opposite. Instead of saving money, it’s adding delays, paperwork, and stress. In 2023, the American Medical Association found that 93% of doctors say prior authorization causes treatment delays. And 24% say those delays have led to hospitalizations.
Why Are Generics Targeted?
You’d think insurers would love generics-they cost 80% less than brand-name drugs and make up 90% of all prescriptions filled. But here’s the twist: insurers aren’t just trying to cut costs. They’re trying to control which generics you get.Many insurance plans have strict formularies. Even if two generics treat the same condition, your plan might only cover one brand-say, Teva’s metformin instead of Mylan’s. If your doctor prescribes the "wrong" generic, you need prior authorization to switch. Sometimes, it’s not about the drug itself-it’s about which manufacturer the pharmacy benefit manager (PBM) has a deal with.
Step therapy is another reason. Insurers make you try a cheaper generic first-even if your doctor knows it won’t work for you. For example, someone with Crohn’s disease might need methotrexate, a generic immunosuppressant. But if your insurer requires you to try three other generics first, you’re stuck waiting. A 2024 study by the Crohn’s & Colitis Foundation found this delay can worsen inflammation, increase flare-ups, and raise long-term costs.
Who’s Doing This-and How Often?
Not all insurers are the same. In 2024, Aetna required prior authorization for 25% of its generic medications. UnitedHealthcare was at 22%. Humana, at 18%. And for certain high-risk generics-like those used in cancer treatment-approval rates jump to 35%.Medicaid programs in 34 states have started limiting or banning prior authorization for common generics. California’s SB 1024, effective January 2025, outright bans it for 47 essential generic drugs on the state’s Essential Drug List. That includes metformin, levothyroxine, and hydrochlorothiazide.
At the federal level, the 2024 Improving Seniors’ Timely Access to Care Act requires Medicare Advantage plans to use electronic prior authorization by 2026 and respond to urgent requests within 72 hours. That’s a step forward. But it doesn’t fix the core problem: the system still treats generics like high-risk drugs.
How It Impacts Real People
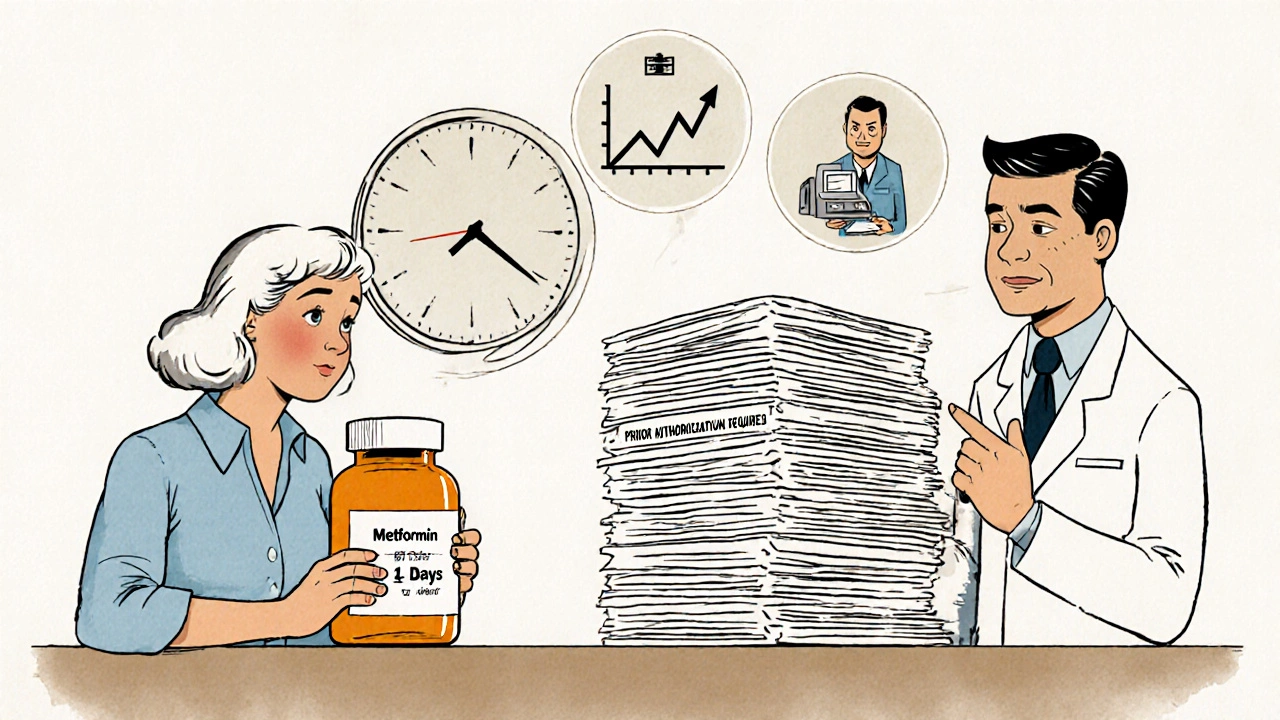
A Kaiser Family Foundation case study followed a patient with type 2 diabetes who needed generic metformin. Her insurance required prior authorization. It took 14 days to get approved. During that time, her blood sugar rose from 6.8% to 8.2%. That’s not just a number-it’s increased risk of nerve damage, kidney problems, and vision loss.On Reddit’s r/healthinsurance, users share stories daily: "My insurance denied my generic thyroid med because they said I needed to try a different brand first." "I had to call my doctor three times just to get a form faxed." "My 82-year-old mom missed her dose because the pharmacy couldn’t get approval in time. She ended up in the ER."
Doctors are drowning in paperwork. One provider on Reddit said their clinic spends 17.3 hours a week just handling prior authorizations for generics. That’s nearly half a full-time employee’s time-time that could be spent diagnosing, treating, or even just listening to patients.
How to Navigate the System
If you’re hit with a prior authorization requirement, don’t panic. Here’s what works:- Ask your doctor to submit electronically. Electronic requests through platforms like CoverMyMeds are 32% faster than fax or phone.
- Request urgent status. If your condition is unstable (like high blood pressure or uncontrolled diabetes), ask your doctor to mark it as urgent. Cigna and others process these within 72 hours.
- Keep records. Save every email, fax confirmation, and phone call. If denied, you can appeal-with documentation.
- Check your formulary. Log into your insurer’s website and search for your medication. See which generic brands are covered without authorization.
- Ask about alternatives. If your preferred generic is blocked, ask your doctor: "Is there another generic on the formulary that’s covered?" Sometimes switching brands solves the issue.
And if your prior authorization is denied? Appeal. The Crohn’s & Colitis Foundation found that 67% of denials are overturned with proper clinical documentation. Your doctor’s note, lab results, or a letter explaining why the first-line generic won’t work can make all the difference.
The Bigger Picture
The real problem isn’t that generics are being blocked. It’s that the system treats them like they’re dangerous or expensive. That’s backwards. Generics are the backbone of affordable care. They save patients billions every year. When insurers make you jump through hoops for them, they’re not saving money-they’re costing more in delayed care, ER visits, and lost productivity.In June 2025, major insurers including Aetna, UnitedHealthcare, and Cigna announced they’d eliminate prior authorization for 12 common generic drug classes by January 2026. That includes ACE inhibitors, statins, and metformin. It’s a win. But it’s only a start. The American Gastroenterological Association says eliminating prior authorization for all first-line generics for chronic conditions would cut total healthcare costs by 18%.
Right now, the system is broken. It’s punishing patients for using cheap, safe drugs. And it’s making doctors into clerks instead of caregivers. The fix isn’t more rules. It’s removing the rules that don’t make sense.
What’s Next?
Federal and state lawmakers are paying attention. The Congressional Budget Office projects a 40% drop in prior authorization requirements for generics by 2028-if current reforms keep moving forward. But until then, patients and providers are stuck in the middle.If you’re affected, speak up. Tell your doctor. Tell your insurer. Tell your state representative. This isn’t just about a pill. It’s about access, dignity, and whether our healthcare system still works for people-or just for paperwork.
Why would my insurance require prior authorization for a generic drug?
Insurers require prior authorization for generics to control which brand or manufacturer they pay for, even if the drug is chemically identical. Sometimes, it’s due to step therapy rules-forcing you to try one generic before another-or because the pharmacy benefit manager has a financial deal with a specific maker. It’s not about safety-it’s about cost control, and often, it’s counterproductive.
Which generic medications commonly require prior authorization?
Common ones include metformin (for diabetes), levothyroxine (for thyroid), lisinopril (for blood pressure), atorvastatin (for cholesterol), and hydrochlorothiazide (a diuretic). High-risk generics like methotrexate (for autoimmune conditions) or certain oncology drugs also face higher approval rates. The list varies by insurer and state.
How long does prior authorization for generics take?
Standard requests take 5-10 business days. Urgent requests should be processed within 72 hours under federal rules for Medicare Advantage plans, but private insurers vary. Some take up to two weeks. Electronic submissions cut approval time by about a third.
Can I appeal a denied prior authorization for a generic?
Yes. About 67% of denials are overturned on appeal if you provide clinical documentation-like lab results, doctor’s notes, or proof of failed alternatives. Your doctor should help you file the appeal. Keep copies of all communication.
Are there states that ban prior authorization for generics?
Yes. California’s SB 1024 (effective January 2025) bans prior authorization for 47 essential generic drugs. Thirty-four other states have restrictions on certain generic classes. Medicaid programs in many states have also eliminated prior authorization for common medications like thyroid and blood pressure generics.
Will this practice go away?
Trends suggest yes. Major insurers agreed in June 2025 to eliminate prior authorization for 12 key generic classes by January 2026. Federal and state reforms are accelerating. The Congressional Budget Office predicts a 40% reduction in generic prior authorizations by 2028. But until then, patients and providers must stay informed and advocate for change.

Write a comment