For decades, leukemia and lymphoma were treated the same way: harsh chemotherapy, long hospital stays, and uncertain outcomes. Today, that’s changing. Targeted therapy and CAR T-cell therapy are no longer experimental - they’re saving lives where traditional treatments failed. Patients who once had months to live are now in remission for years, sometimes indefinitely. This isn’t science fiction. It’s happening right now in hospitals across North America, including in Vancouver, Toronto, and Seattle.
What Targeted Therapies Actually Do
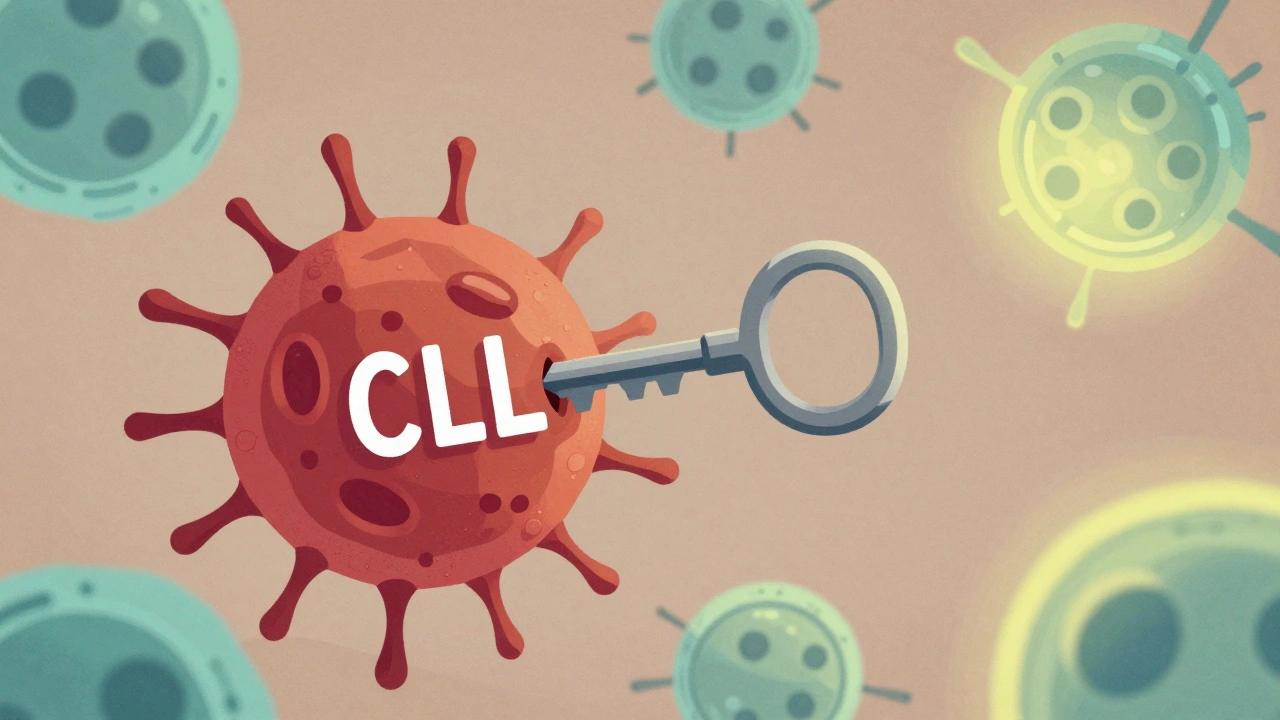
Targeted therapies don’t attack all fast-growing cells like chemo does. They zero in on specific proteins or signals that cancer cells rely on to survive. Think of it like cutting the power to a single machine in a factory, instead of shutting down the whole plant. For chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL), two of the most common types, BTK inhibitors like ibrutinib and acalabrutinib have become standard. These drugs block a protein called Bruton’s tyrosine kinase - a key signal that tells cancer cells to keep multiplying. Patients take them as pills, once a day. No IVs. No nausea. Many keep working, traveling, even hiking after starting treatment. Then there’s venetoclax, a BCL-2 inhibitor. It wakes up a built-in self-destruct switch inside cancer cells. Used with the antibody obinutuzumab, it’s given in fixed 12-month courses. After that, many patients stop treatment entirely - something unthinkable with chemo. In clinical trials, over 70% of patients had no detectable cancer in their blood after one year. These aren’t just minor improvements. A 2025 study from the CLL Society showed that patients on targeted therapies took nearly five years before their disease transformed into a more aggressive form (called Richter transformation), compared to just 2.2 years with old-school chemo. That’s a massive delay in disease progression.CAR T-Cell Therapy: Rewiring the Immune System
If targeted therapy is like a sniper, CAR T-cell therapy is like training your own army to hunt down cancer. Here’s how it works: First, doctors pull blood from the patient and isolate their T cells - the immune system’s frontline fighters. These cells are sent to a lab, where scientists add a special receptor - a chimeric antigen receptor, or CAR - that lets them recognize CD19, a protein found on nearly all B-cell lymphomas and leukemias. The modified cells are grown in large numbers, then infused back into the patient. It sounds complex, and it is. But the results? Stunning. In relapsed or refractory mantle cell lymphoma, one CAR T therapy called LV20.19 achieved a 100% response rate in a 2025 trial. Eighty-eight percent of patients had no detectable cancer left after treatment. Three CAR T therapies are FDA-approved as of 2025: tisagenlecleucel (Kymriah), axicabtagene ciloleucel (Yescarta), and lisocabtagene maraleucel (Breyanzi). Yescarta, for example, showed a 42.6% four-year survival rate in patients with large B-cell lymphoma who had already failed other treatments - a number that would have been under 10% just a decade ago. Newer versions are even more advanced. Gilead’s KITE-363 and KITE-753 target both CD19 and CD20 at the same time. Why? Because cancer cells sometimes stop making CD19 to escape treatment. By hitting two targets, these next-gen therapies reduce the chance of relapse. Early data from ASH 2025 shows a 63.6% complete remission rate in patients who had exhausted all other options.Why These Therapies Aren’t for Everyone
These treatments are powerful - but they’re not magic bullets. Targeted therapies can stop working. Many patients on ibrutinib see their cancer return after 3 to 5 years. Those with TP53 or del(17p) mutations tend to respond less well and progress faster. When one drug fails, doctors try another - but eventually, resistance builds. That’s why combinations are now the focus: venetoclax + ibrutinib, for instance, can push remissions deeper and longer. CAR T-cell therapy has its own hurdles. About 20-40% of patients develop neurotoxicity - confusion, tremors, or seizures. Another 50-80% experience cytokine release syndrome (CRS), a dangerous immune overreaction that can spike fevers, drop blood pressure, and require ICU care. Managing these side effects demands specialized teams, 24/7 monitoring, and access to drugs like tocilizumab. And then there’s the wait. Manufacturing a patient’s own CAR T cells takes 3 to 5 weeks. For someone with aggressive lymphoma, that’s a long time to wait. Some patients get worse while waiting. That’s why researchers are now testing “off-the-shelf” CAR T cells from healthy donors - but those are still in trials.
Cost, Access, and the Real-World Gap
The price tag for CAR T-cell therapy is $373,000 to $475,000 per treatment. Even with insurance, patients often face $15,000 to $25,000 in out-of-pocket costs per month for targeted drugs. That’s not just financial stress - it’s a barrier to care. In Canada, access varies by province. While major centers like BC Cancer in Vancouver offer CAR T-cell therapy, many community oncologists don’t have the infrastructure. Only 32% of community practices in the U.S. can deliver CAR T, compared to 89% of NCI-designated cancer centers. That means rural patients often have to travel hundreds of miles - and take time off work - just to get treated. There’s also a learning curve. Doctors need training to manage CRS, interpret minimal residual disease (MRD) tests, and decide when to switch therapies. The American Society of Hematology says it takes 6 to 12 months for a new team to become proficient. That delay means some patients miss their window for the best treatment.What’s Next? The Future Is Already Here
The next wave of therapies is moving faster than ever. In 2025, the FDA gave priority review to lisocabtagene maraleucel for marginal zone lymphoma - a rare subtype that had few options. Approval is expected by December 2025. Researchers are also testing CAR T-cell therapy earlier - not just after multiple relapses, but as a first-line option for high-risk patients. A 2025 ASCO survey found that 68% of hematologists believe CAR T will become standard first-line treatment for certain lymphomas by 2030. Meanwhile, dual-target CAR T cells, gene-edited T cells, and even CAR NK (natural killer) cells are entering trials. One early study in Nature showed autologous stem cell transplant is now being used upfront for some mantle cell lymphoma patients - a shift from just a few years ago, when transplant was only for the very young. And while targeted therapies still dominate (used in 85% of eligible CLL patients), CAR T-cell use is growing. In 2025, 33 new non-genetically modified cell therapy trials were launched - up from 27 the previous quarter. Most are focused on solid tumors, but blood cancer remains the core.
What Patients Should Know Right Now
If you or someone you know has leukemia or lymphoma, here’s what matters:- Ask about genetic testing - mutations like TP53 or del(17p) change your treatment options.
- Don’t assume chemo is your only choice. Targeted drugs like venetoclax and ibrutinib are now first-line for many.
- If you’ve relapsed, ask if CAR T-cell therapy is an option. It’s not just for last-resort cases anymore.
- Find a center with experience. CAR T requires a team - not just an oncologist, but nurses, neurologists, and ICU staff trained in managing toxicity.
- Understand the cost. Talk to social workers. Some manufacturers offer patient assistance programs that can cut out-of-pocket costs by 70%.
When to Consider Clinical Trials
Even with all these advances, not everyone responds. That’s where trials come in. Over 500 active trials are testing new combinations, next-gen CAR T cells, and oral alternatives to infusions. Many are recruiting patients who’ve tried two or more therapies. If your doctor hasn’t mentioned a trial, ask. Trials aren’t just for people with no options - they’re often where the most effective new treatments are first tested.Final Thoughts
Leukemia and lymphoma are no longer automatic death sentences. The tools we have now - targeted pills, reprogrammed immune cells - are turning chronic diseases into manageable conditions, and in some cases, curing them. But these advances aren’t automatic. They require awareness, access, and advocacy. The best outcomes come when patients ask questions, seek second opinions, and connect with centers that specialize in these therapies. The future of blood cancer care isn’t just better drugs - it’s smarter, more personalized, and more human care.Are targeted therapies better than chemotherapy for leukemia and lymphoma?
Yes, for most patients with CLL, SLL, and many types of lymphoma. Targeted therapies like BTK and BCL-2 inhibitors work more precisely, cause fewer side effects like hair loss and severe infections, and often allow patients to avoid hospital stays. Studies show they improve progression-free survival by 2 to 3 times compared to older chemoimmunotherapy regimens.
How long does CAR T-cell therapy take from start to finish?
The entire process takes 4 to 8 weeks. First, you undergo leukapheresis to collect your T cells - that’s a single day. Then, the cells are shipped to a lab and genetically modified, which takes 3 to 5 weeks. Once they’re ready, you receive conditioning chemo for 2-3 days, followed by the CAR T infusion. After that, you stay near the treatment center for at least 2 weeks for monitoring. Some patients need longer if they develop side effects like cytokine release syndrome.
Can you get CAR T-cell therapy more than once?
It’s possible, but rare. Most patients who relapse after CAR T don’t get a second infusion because their T cells may be too damaged or the cancer may have changed. Instead, doctors turn to other options - new targeted drugs, clinical trials, or stem cell transplants. Some newer CAR T designs are being tested for re-treatment, but that’s still experimental.
What are the biggest side effects of CAR T-cell therapy?
The two main dangers are cytokine release syndrome (CRS) and neurotoxicity. CRS causes high fever, low blood pressure, and trouble breathing - it usually happens within the first week. Neurotoxicity can lead to confusion, trouble speaking, seizures, or loss of coordination. Both require immediate medical care. About 20-40% of patients experience neurotoxicity, and 50-80% have some level of CRS. Most cases are manageable with drugs like tocilizumab and steroids.
Is CAR T-cell therapy available in Canada?
Yes, but only at specialized centers. In Canada, CAR T-cell therapy is available at BC Cancer in Vancouver, Princess Margaret Cancer Centre in Toronto, and the Montreal Cancer Institute. Not all hospitals offer it - it requires ICU-level care, specialized labs, and trained staff. Access varies by province and insurance coverage, but most public plans cover approved therapies for eligible patients.
How do you know if a targeted therapy is working?
Doctors use blood tests to check for cancer cells, especially minimal residual disease (MRD) testing. This can detect one cancer cell in a million normal cells. If MRD becomes undetectable after treatment, it’s a strong sign the therapy is working deeply. Imaging scans like PET-CT also help track lymph node shrinkage. Most patients see improvement in blood counts and symptoms within weeks.
Do targeted therapies cure leukemia and lymphoma?
Some do - but not always. For certain patients with CLL or lymphoma, combinations like venetoclax + ibrutinib can lead to long-term remission - so long that doctors call it a functional cure. CAR T-cell therapy has cured some patients with multiply relapsed disease who had no other options. But for many, these therapies control the disease rather than eliminate it entirely. Ongoing monitoring is still needed.

Write a comment