Many mothers worry that taking medication while breastfeeding will harm their baby. The truth? 98% of medications are safe to use while nursing - if you time them right. It’s not about avoiding medicine altogether. It’s about working with your body’s natural rhythms to keep your baby safe while you stay healthy.
Why Timing Matters More Than You Think
Medication doesn’t just disappear after you swallow it. It enters your bloodstream, then slowly moves into your breast milk. The amount your baby gets depends on when you take the pill versus when they feed. That’s why timing isn’t just helpful - it’s critical.Think of it like this: when you take a medication, your blood levels rise to a peak, then fall. Breast milk follows that same curve. If you nurse right after taking a pill, your baby gets the highest dose. But if you nurse right before, the drug hasn’t had time to build up yet. That small shift can cut infant exposure by half - or more.
The science behind this isn’t new. Studies from the 1980s showed that drug transfer into milk follows predictable patterns. Today, guidelines from the American Academy of Pediatrics, the Academy of Breastfeeding Medicine, and the CDC all agree: timing can make a real difference.
How to Time Single-Dose Medications
If you’re taking a medication once a day - like a painkiller or an antidepressant - the best strategy is simple: take it right before your baby’s longest stretch of sleep.Most babies sleep 6 to 8 hours at night. That’s your window. Take your pill right after the bedtime feeding. By the time your baby wakes up, the drug concentration in your milk has dropped significantly. For example:
- Hydrocodone peaks in your blood at 0.5 to 2 hours after taking it. Half-life: 3-4 hours. Nurse before the dose, and your baby gets far less.
- Oxycodone peaks in 0.5-2 hours. Half-life: 3-4 hours. Same rule applies.
- Alprazolam (immediate-release) peaks at 1-2 hours. Half-life: 11 hours. Nurse before the dose. Avoid extended-release versions - they spike later and are harder to time.
One mother in Los Angeles, whose baby was born prematurely, used this exact method with hydrocodone after a C-section. She pumped and stored milk before her first dose, then fed the stored milk for the next 4 hours. She resumed nursing normally after that. Her baby showed no signs of drowsiness or feeding issues.
What to Do With Multiple Daily Doses
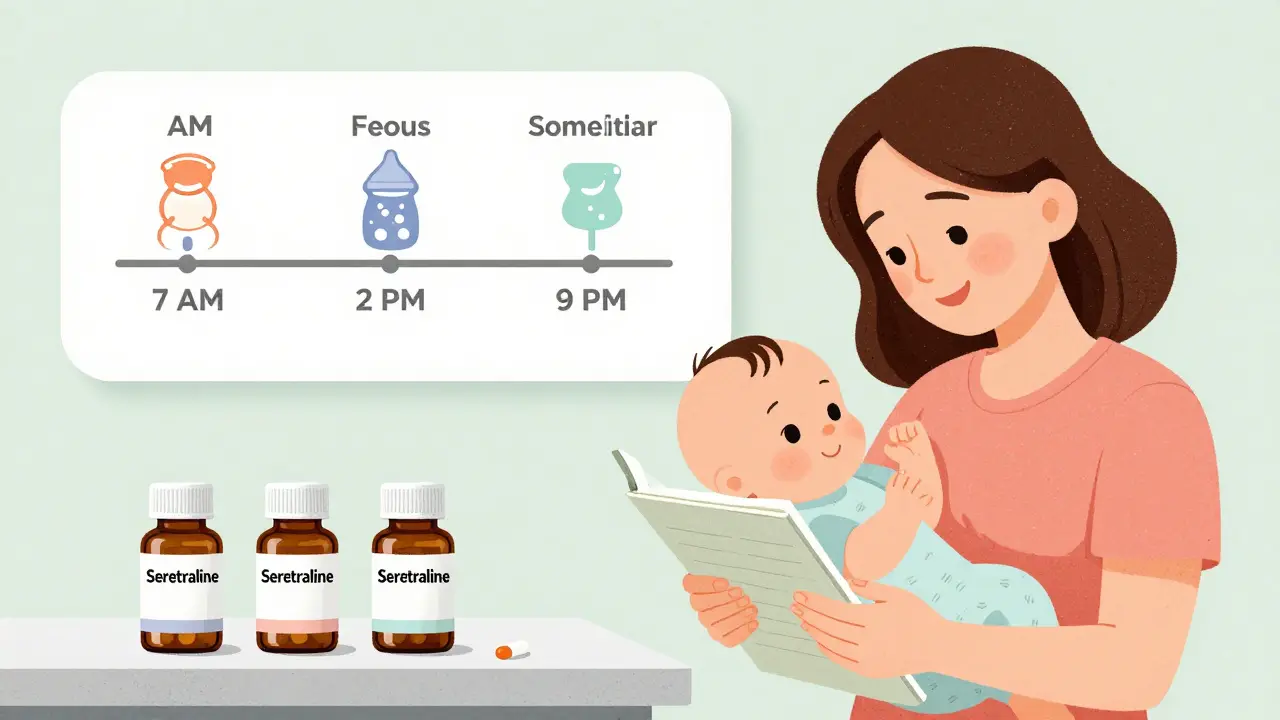
If you need to take your medication two or three times a day - common for antibiotics, thyroid meds, or psychiatric drugs - the rule is even simpler: nurse immediately before each dose.This works because your milk levels are lowest right before you take the next pill. By feeding right before, you’re using the natural dip in drug concentration. After you take the pill, your milk levels rise, but by the next feeding (usually 3-4 hours later), they’ve already started to fall again.
For example:
- Sertraline (an SSRI) has a 26-hour half-life. It builds up slowly. Nursing before each dose keeps infant exposure low - and studies show it’s one of the safest SSRIs for breastfeeding.
- Fluoxetine has a 96-hour half-life. Its active metabolite lasts over 260 hours. Even with timing, it accumulates. Experts recommend avoiding it if possible. Sertraline or paroxetine are better choices.
- Prednisone at standard doses is fine. But if you’re on a high dose (over 20 mg daily), wait 4 hours after taking it before nursing. The amount in milk drops sharply after that.
Which Medications Are Riskiest - and Why
Not all drugs are created equal. Some are easy to time. Others? Not so much.Long half-life drugs are the biggest challenge. A half-life is how long it takes for half the drug to leave your body. If it’s longer than 24 hours, timing barely helps because the drug is always in your system.
- Diazepam has a half-life of 44-48 hours. Even if you nurse right before taking it, the drug lingers. Infants have been reported to become excessively sleepy or have feeding problems. Avoid if possible. If you must use it, consider lorazepam instead - it has a shorter half-life (10-20 hours) and lower transfer into milk.
- Lorazepam peaks in 1-2 hours, half-life under 20 hours. Relative Infant Dose (RID) is just 2.6-2.9%. Much safer for timing.
- Alprazolam extended-release peaks at 9 hours. That’s a nightmare for timing. Stick to immediate-release.
For opioids, the CDC recommends never exceeding 30 mg of hydrocodone per day. Always nurse before dosing. Watch your baby for signs of sedation: unusual sleepiness, poor sucking, slow breathing. If you see any, contact your pediatrician.
Special Cases: Newborns, Preemies, and High-Risk Babies
The younger the baby, the higher the risk. Newborns and preemies don’t process drugs the way older babies do. Their livers and kidneys are still developing. That means even small amounts of medication can stick around longer in their systems.Mayo Clinic specialists warn that timing is especially crucial for babies under 6 weeks old. After that, their ability to clear drugs improves dramatically. So if your baby is 3 months old and you’re on a short-acting medication, you have more flexibility.
For preemies or babies with kidney or liver issues, consider:
- Pumping and dumping before a dose, then feeding stored milk.
- Choosing medications with the lowest RID (below 10%).
- Monitoring for irritability, poor weight gain, or sleep changes.
A 2022 survey of 157 lactation consultants found that 87% of mothers successfully timed hydrocodone, but only 42% could manage diazepam without issues. The difference? Half-life. Simple math. Long half-life = hard to time.
Tools and Resources You Can Trust
You don’t have to guess. There are reliable, free tools that give you exact timing advice for over 4,700 medications.- LactMed - Updated monthly by the U.S. National Library of Medicine. Search any drug and get details on peak times, half-life, RID, and recommended timing. It’s free at toxnet.nlm.nih.gov (no login needed).
- Hale’s Medication and Mothers’ Milk - The gold standard reference. Uses the RID system. Anything under 10% is generally safe. Over 10%? Proceed with caution.
- LactMed App - Available for iOS and Android. Over 127,000 users as of 2023. Syncs with your feeding schedule.
Many hospitals now use these tools in their lactation consultations. If your doctor doesn’t know about them, ask for a referral to a lactation consultant. They’re trained in this exact thing.
What About Hormonal Birth Control?
Combination birth control pills (estrogen + progestin) are not recommended in the first 3-4 weeks after birth. Estrogen can reduce milk supply. The AAFP says wait at least 3 weeks. Some experts say 4-6 weeks, especially if your supply is still building.Progestin-only pills (the mini-pill) are safe to start sooner. They don’t affect supply as much. Timing isn’t critical here - the dose is low and steady. Just take it at the same time every day.

Real-Life Success Stories
One mother in Ohio, on sertraline for postpartum depression, was terrified she’d have to stop breastfeeding. Her doctor told her to nurse right before each dose - morning, afternoon, and night. She kept a feeding log. After two weeks, her baby was thriving. Her mood improved. She’s still breastfeeding at 14 months.Another mother had dental surgery and needed hydrocodone. She pumped 8 ounces before the procedure. Fed that milk for the next 4 hours. Then resumed nursing. Her 6-month-old showed no signs of drowsiness. She posted about it on r/breastfeeding: "It worked better than I hoped. I felt in control."
Common Mistakes to Avoid
Even with good intentions, people mess up. Here’s what not to do:- Don’t wait to nurse until after the pill - that’s when milk levels are highest.
- Don’t assume "natural" means safe - herbal supplements like valerian or kava can be just as risky as prescription drugs.
- Don’t use extended-release versions unless your provider says it’s okay. They’re harder to time.
- Don’t skip doses - untreated depression, infection, or pain can hurt your ability to care for your baby more than the medication ever could.
And remember: if you’re unsure, pump and dump once. Store milk before your dose. Feed it to your baby during the peak window. Then resume normal feeding. It’s not perfect - but it’s safe.
What’s Changing in 2026?
The FDA now requires all new drugs to include specific breastfeeding data - including timing recommendations - before approval. By 2025, every new medication label will have this info. That’s a big win.Researchers are also studying how individual differences - like milk fat content or pH - affect drug transfer. Early data shows some women transfer up to 300% more of certain drugs than others. Personalized timing might be the next step.
For now, stick to the proven method: know your drug’s half-life. Nurse before the dose. Use LactMed. Talk to your provider. And don’t let fear stop you from getting the care you need.
Can I breastfeed after taking painkillers like ibuprofen or acetaminophen?
Yes. Both ibuprofen and acetaminophen are safe during breastfeeding. They transfer in very small amounts (RID under 1%). You don’t need to time them precisely. Take them as needed, even right after nursing. They’re among the safest options.
Is it safe to breastfeed after taking antibiotics?
Most antibiotics are safe. Penicillin, amoxicillin, cephalexin, and clindamycin all have low transfer into milk. Nurse before your dose to minimize exposure. Watch your baby for diaper rash or fussiness - signs of a gut imbalance. If you see either, talk to your pediatrician. Probiotics can help.
What if my baby is premature? Should I avoid all medications?
No. Premature babies can still benefit from breastfeeding, even with medication. But timing is more important. Use the lowest effective dose. Choose medications with short half-lives and low RID. Pump and store milk before dosing if you’re unsure. Always consult a neonatologist or lactation specialist familiar with preemies.
Can I use CBD or marijuana while breastfeeding?
No. THC, the active ingredient in marijuana, stays in breast milk for days and can affect brain development. Even if you time it, it doesn’t clear quickly enough. The AAP and CDC strongly advise against using marijuana while breastfeeding. There is no safe timing strategy.
Do I need to pump and dump after taking medication?
Only if you’re on a medication with a very long half-life (like diazepam) or if you’re unsure about safety. For most medications, pumping and dumping isn’t necessary. Timing your feedings is far more effective. Pumping and dumping just reduces your supply - and doesn’t speed up drug clearance from your body.
How do I know if my baby is affected by my medication?
Watch for changes: excessive sleepiness, poor feeding, irritability, slow weight gain, or breathing problems. If your baby seems different after you start a new medication, contact your pediatrician. Keep a log: note the time you took the drug, when you nursed, and how your baby acted. That helps your doctor decide if it’s the medication.


Write a comment