GAHT Drug Interaction Checker
Interaction Results
Select your GAHT type and medication category to see potential interactions.
When someone starts gender-affirming hormone therapy (GAHT), they’re not just changing their body-they’re changing how their body processes everything else. Estradiol, testosterone, anti-androgens, and GnRH agonists don’t exist in a vacuum. They interact with medications people are already taking-for HIV, depression, anxiety, high blood pressure, and more. These interactions aren’t theoretical. They’re real, measurable, and can change how well your treatment works-or put your health at risk.
How GAHT Works and Why Interactions Matter
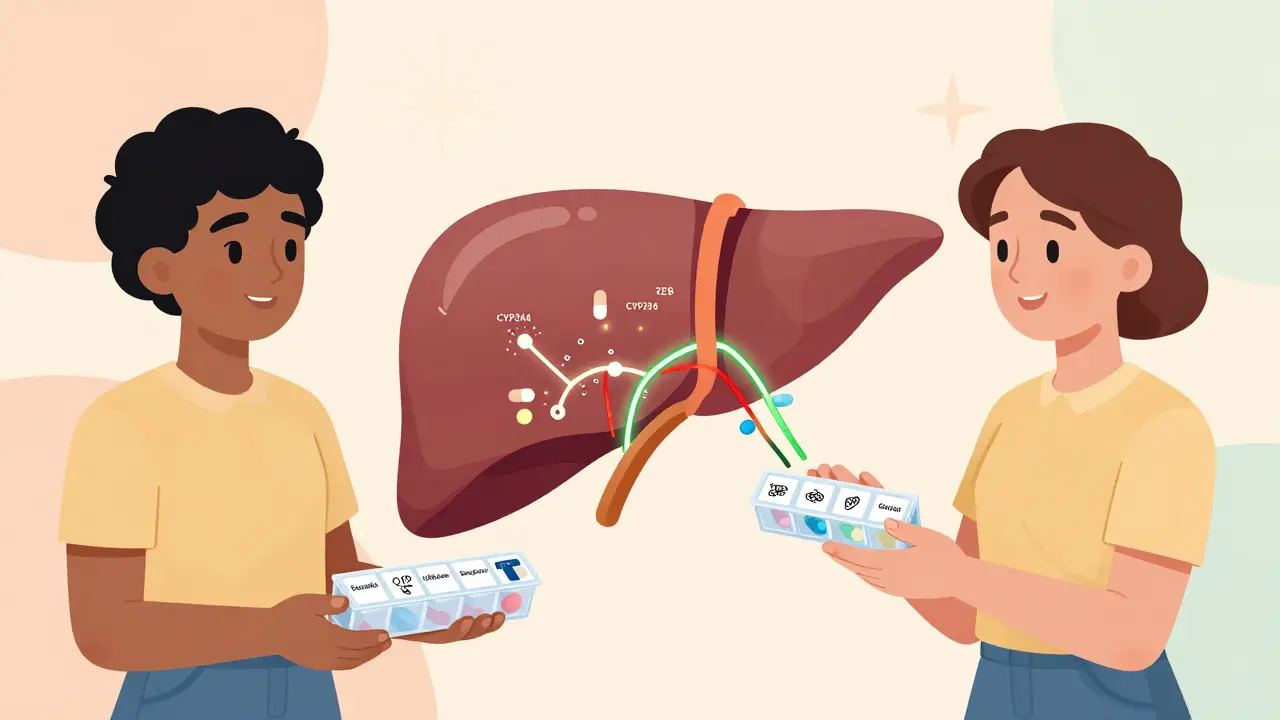
Gender-affirming hormone therapy falls into two main types: feminizing (FHT) and masculinizing (MHT). FHT usually means estradiol-taken as patches, pills, or injections-along with an anti-androgen like spironolactone or cyproterone acetate to block testosterone. MHT means testosterone, delivered as gels, injections, or pellets. These hormones don’t just affect your skin, voice, or muscle mass. They’re metabolized by specific liver enzymes, especially CYP3A4 and CYP2D6. That’s where problems start.
Many common drugs either speed up or slow down these enzymes. If your body breaks down estradiol faster, your hormone levels drop. You might lose the benefits of your therapy: less breast development, mood swings returning, or fatigue. If it breaks it down slower? Estradiol builds up. That raises your risk of blood clots, stroke, or liver issues. The same goes for testosterone. It’s processed by 5-alpha reductase and aromatase. Some drugs interfere with those pathways too.
And here’s the thing: transgender people are more likely to be on other medications. The 2021 National Transgender Survey found that 2.5 times more transgender people live with depression or anxiety than cisgender people. Rates of HIV are 3.4 times higher. That means many people on GAHT are also on antidepressants, antiretrovirals, or PrEP. These combinations aren’t rare. They’re common. And they need careful management.
Antiretrovirals and GAHT: A High-Stakes Mix
If you’re living with HIV and on antiretroviral therapy (ART), your hormone levels can shift dramatically depending on what you’re taking. The biggest red flag? Enzyme-inducing drugs like efavirenz (600 mg daily). Studies show these can slash estradiol levels by 30% to 50%. That’s not a small drop. It’s enough to make your feminizing therapy ineffective. You might feel like you’re backsliding-no breast growth, mood crashes, hot flashes returning. That’s not in your head. It’s in your liver.
On the flip side, some HIV meds do the opposite. Cobicistat-boosted regimens-like darunavir/cobicistat (800/150 mg daily)-block the enzymes that break down estradiol. That causes estradiol to pile up. One study found levels jumped 40% to 60% within two weeks. That’s dangerous. Higher estradiol means higher risk of blood clots. The American Heart Association says estradiol above 200 pg/mL increases clotting risk in women over 35. For transgender women, hitting that level isn’t unusual when paired with cobicistat.
Good news? Integrase inhibitors like dolutegravir (50 mg daily) don’t interfere much. They may raise estradiol by 25% to 35%, but that’s usually safe and doesn’t require dose changes. And GnRH agonists like leuprolide? They don’t interact with any ART. That’s one less thing to worry about.
For PrEP, the data is even more reassuring. A 2022 study of 172 transgender people on tenofovir/emtricitabine (TDF/FTC) showed no meaningful change in hormone levels. Tenofovir levels stayed stable too. That means you can take PrEP and GAHT together without adjusting either. No extra pills. No extra risks. Just safe, effective protection.
Psychiatric Medications: The Hidden Risk
Depression, anxiety, PTSD-these are common among transgender people. So are SSRIs like fluoxetine, sertraline, or escitalopram. Here’s where things get messy. Some SSRIs inhibit CYP2D6, the same enzyme that helps clear estradiol. That means estradiol sticks around longer. Levels can rise by 20% to 30%. That’s not always bad-but it’s unpredictable. You might feel better emotionally… or you might feel dizzy, nauseous, or swollen. That’s not just "side effects." It’s a drug interaction.
Worse are mood stabilizers like carbamazepine or phenytoin. These are strong CYP3A4 inducers. They speed up estradiol breakdown. Studies show they can cut hormone levels by up to 40%. If you’re on carbamazepine for bipolar disorder and start GAHT, you might need a higher dose of estradiol just to get the same results. And if you stop the mood stabilizer later? Your estradiol levels could spike. That’s a risk no one wants to discover after a hospital visit.
Testosterone doesn’t play nice either. A 2023 review found 17 cases where people on testosterone saw their antidepressants stop working. Their mood dropped. Their anxiety spiked. Doses had to be increased by 25% to 50% within six weeks. That’s not a coincidence. Testosterone changes how your brain metabolizes serotonin. And most antidepressants were never tested on people on testosterone. The clinical trials? Only 3% included transgender participants. So we’re guessing. And guessing with mental health is dangerous.
What About Blood Thinners, Diuretics, or Blood Pressure Meds?
Spironolactone, a common anti-androgen in FHT, is also a diuretic. That means it can interact with other diuretics, ACE inhibitors, or NSAIDs like ibuprofen. Taking them together can spike potassium levels. High potassium can cause heart rhythm problems-even cardiac arrest. If you’re on spironolactone, you need regular blood tests to check potassium. Every 3 months, at least.
And if you’re on blood thinners like warfarin? Estradiol can make them more potent. That means you bleed easier. INR levels can rise unexpectedly. You’ll need more frequent checks. Same with statins. Estradiol can raise levels of some statins, increasing the risk of muscle damage. Your doctor needs to know everything you’re taking-prescription, over-the-counter, supplements.
Even common things like St. John’s wort or grapefruit juice matter. St. John’s wort induces CYP3A4. It can tank your estradiol levels. Grapefruit juice blocks it. That can cause estradiol to build up. You might not think of them as "medications," but they are. And they’re not safe to mix.
What Should You Do? A Practical Guide
You don’t need to panic. But you do need to be proactive. Here’s what works:
- Make a full list-every pill, patch, supplement, herb, and OTC med you take. Include vitamins, CBD, melatonin, and birth control you took before transition.
- Bring it to every appointment. Don’t assume your provider knows. Only 41% of U.S. endocrinology clinics have standardized screening. You might be the only one who knows your full med list.
- Ask about CYP3A4 and CYP2D6. If your doctor doesn’t know these terms, ask for a pharmacist. Clinical pharmacists who specialize in transgender care are your best ally.
- Get blood tests. Monitor estradiol, testosterone, potassium, liver enzymes, and lipids every 3 months in the first year. After that, every 6 months. If you start a new med, test again in 4 weeks.
- Track your symptoms. Did your mood change after starting a new antidepressant? Did your breast tenderness disappear after switching HIV meds? Write it down. That’s data your provider needs.
And if you’re on PrEP? Keep taking it. It’s safe. If you’re on ART? Don’t delay GAHT-but do coordinate timing. Start ART first if you can. Let your viral load stabilize before starting hormones. That gives your body a better chance to adjust.
The Future Is Getting Better-But Not There Yet
Research is catching up. The NIH’s Tangerine Study, running through 2025, is tracking 300 transgender adults on GAHT and 12 psychiatric drugs. Preliminary results will come in early 2025. That’s huge. For the first time, we’ll have real data on how sertraline or bupropion interacts with testosterone.
Pharmaceutical companies are finally listening. Gilead Sciences now requires GAHT interaction testing in all new PrEP trials. The FDA is pushing for more inclusive clinical trials. That’s progress.
But gaps remain. We still don’t know how cabotegravir (the long-acting PrEP shot) interacts with hormones. Or how brexanolone (a postpartum depression drug) affects testosterone. There are only two published case reports on those combinations. That’s not enough.
What we do know is this: GAHT is safe. It’s effective. But it’s not simple. It doesn’t work the same way for everyone. And it doesn’t play well with every other drug. The key isn’t avoiding treatment. It’s managing it with knowledge, vigilance, and support.
If you’re on GAHT and another medication, don’t guess. Don’t assume. Don’t wait until something goes wrong. Talk to your provider. Ask for a pharmacist. Get tested. Keep a log. Your body is changing. Make sure your meds are working with it-not against it.
Can I take PrEP while on gender-affirming hormones?
Yes. A 2022 study of 172 transgender people on tenofovir/emtricitabine (TDF/FTC) PrEP showed no clinically significant changes in hormone levels or PrEP effectiveness. Hormone concentrations stayed within normal ranges, and tenofovir levels remained protective. You do not need to adjust your PrEP dose. This combination is safe and recommended.
Does testosterone interfere with antidepressants?
Yes, it can. In 17 documented cases, people on testosterone experienced reduced effectiveness of their antidepressants, leading to worsening depression or anxiety. Dose increases of 25% to 50% were often needed within six weeks. This isn’t universal-but it’s common enough that anyone starting testosterone should be monitored closely for mood changes, especially in the first 3 months.
Can HIV meds make my estrogen therapy stop working?
Absolutely. Enzyme-inducing HIV drugs like efavirenz can reduce estradiol levels by 30% to 50%, making feminizing therapy less effective. You might notice less breast development, increased body hair, or mood swings returning. If you’re on efavirenz or similar drugs, your provider should switch you to a non-interacting regimen like dolutegravir or monitor your estradiol levels closely.
Is it safe to take birth control with GAHT?
For transgender women, estrogen-based birth control is unnecessary and potentially dangerous. It adds extra estrogen, increasing clotting risk. For transgender men, progestin-only pills or IUDs are safer than combined pills, which can interfere with testosterone’s effects. Always consult your provider before using any hormonal contraception with GAHT.
What should I do if I start a new medication?
Stop and consult your provider before starting anything new-even OTC meds or supplements. Ask: "Does this affect CYP3A4 or CYP2D6?" Get your hormone levels checked 4 weeks after starting the new drug. Track any changes in mood, energy, swelling, or side effects. Don’t assume it’s "just a side effect." It could be an interaction.
Knowing how your hormones interact with other drugs isn’t about fear. It’s about control. You’re not just surviving transition-you’re thriving. And that means managing every part of your health with care, clarity, and confidence.

Write a comment