Millions of people deal with fungal infections every year, but most don’t know the difference between athlete’s foot and a yeast infection. They’re both caused by fungi, sure-but they behave differently, show up in different places, and need different treatments. If you’ve ever had that itchy, peeling skin between your toes or a persistent vaginal itch, you’re not alone. And if you’ve tried an over-the-counter cream and it came back a few weeks later, you’re not failing-you’re just missing key facts.
What Exactly Is Causing Your Infection?
Fungi are everywhere. They live in soil, on plants, and even on your skin. Normally, your immune system and good hygiene keep them in check. But when conditions get warm, moist, and dark-like inside sweaty shoes or under a damp towel-they start to grow out of control.
There are two main types of fungal infections you’re likely to encounter: dermatophytes and Candida. Dermatophytes are the fungi behind athlete’s foot, jock itch, and ringworm. They feed on keratin-the tough protein in your skin, hair, and nails. Candida, on the other hand, is a yeast. The most common type, Candida albicans, lives naturally in your mouth, gut, and vaginal area. It only becomes a problem when it multiplies too fast.
Here’s the thing: athlete’s foot and yeast infections aren’t the same disease. Mixing them up leads to wrong treatments. Using a cream meant for athlete’s foot on a yeast infection won’t work. And vice versa.
Athlete’s Foot: More Common Than You Think
Athlete’s foot, or tinea pedis, affects about 15% of people worldwide at any given time. In warm, humid climates, that number jumps to 25-30%. It’s not just athletes-anyone who walks barefoot in locker rooms, public showers, or pool decks is at risk. The fungus spreads through skin flakes left on floors, towels, or shoes.
There are three main types:
- Interdigital (70% of cases): Peeling, cracking, and itching between the toes-especially between the fourth and fifth toes.
- Moccasin type (20%): Dry, flaky skin covering the soles and sides of the feet. Often mistaken for eczema.
- Vesicular/bullous (10%): Small blisters filled with fluid, usually on the bottom of the foot.
Here’s what most people get wrong: athlete’s foot doesn’t go away on its own. Even if the itching stops after a few days of cream, the fungus is still there. Stopping treatment early is the #1 reason it comes back. Studies show that 40% of people who quit treatment before finishing get a recurrence within a year.
Candida: When Your Body’s Normal Fungi Turn Against You
While athlete’s foot is a skin problem, Candida can affect your mouth, throat, genitals, and even your bloodstream. About 75% of women will have at least one vaginal yeast infection in their lifetime. Oral thrush-white patches in the mouth-is common in babies, older adults, and people with weakened immune systems.
People with diabetes, HIV, or those taking antibiotics or corticosteroids are more likely to get Candida overgrowth. Antibiotics kill off good bacteria that normally keep yeast in check. That’s why some women get yeast infections after a round of antibiotics for a sinus infection.
Invasive candidiasis-when the fungus enters the bloodstream-is rare but dangerous. The CDC reports about 46,000 cases in the U.S. each year, with a mortality rate as high as 40% in immunocompromised patients. That’s why doctors treat it aggressively with oral or IV antifungals.
How Antifungal Treatments Actually Work
Not all antifungal creams are the same. The most common ones fall into two categories: azoles and allylamines.
- Azoles (clotrimazole, miconazole): Stop fungi from making cell membranes. They’re in most OTC creams. Effective for mild cases, but slower. Takes 2-4 weeks to clear.
- Allylamines (terbinafine): Kill fungi directly. Faster and more effective. Studies show terbinafine cream clears athlete’s foot in 10-14 days, compared to 3-4 weeks for clotrimazole.
One underrated option is Whitfield’s ointment-a mix of 3% salicylic acid and 6% benzoic acid. It doesn’t just kill fungus; it gently peels off the dead, infected skin layer. DermNet NZ studies found it cleared 65% of interdigital athlete’s foot cases in four weeks-better than clotrimazole alone.
For stubborn cases, oral meds are needed:
- Terbinafine (250 mg daily for 2-6 weeks): 85% cure rate for athlete’s foot.
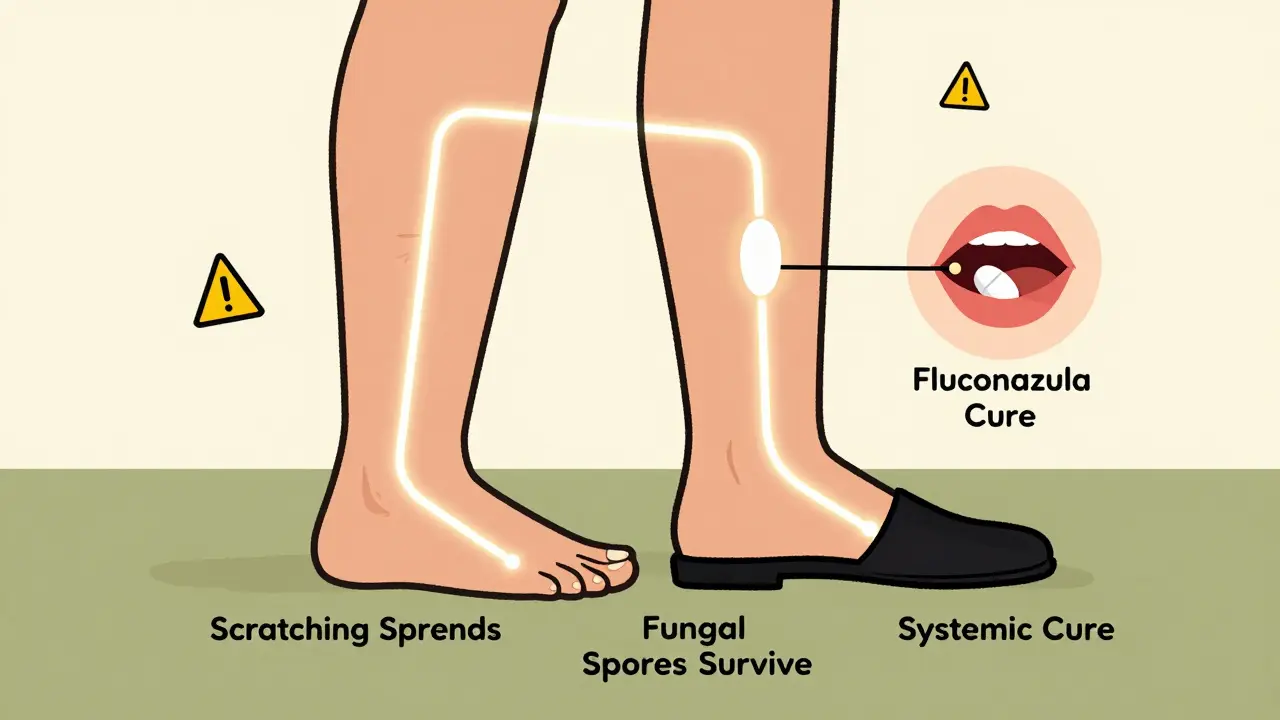
- Fluconazole (150 mg weekly for 2-4 weeks): First-line for vaginal yeast infections.
- Itraconazole (200 mg daily for 1-2 weeks): Used for nail infections or resistant cases.
Oral antifungals have higher cure rates and lower recurrence-only 15-20% come back versus 40% with topical-only treatment. But they’re not for everyone. They can affect the liver, so your doctor will check your blood work first.
What Works Best? Real-World Results
Looking at user reviews and clinical data, here’s what actually works:
| Treatment | Best For | Time to Relief | Cure Rate | Recurrence Rate |
|---|---|---|---|---|
| Terbinafine cream | Athlete’s foot (interdigital) | 48-72 hours | 85% | 18% |
| Clotrimazole cream | Mild athlete’s foot, yeast infections | 5-7 days | 70% | 40% |
| Fluconazole (oral) | Vaginal yeast infection | 24-48 hours | 90% | 15% |
| Whitfield’s ointment | Thick, peeling skin (moccasin type) | 7-10 days | 65% | 22% |
One Reddit user, ‘FootFungusFighter’, shared: “Clotrimazole failed for 3 weeks. Terbinafine cream cleared my 6-month case in 10 days.” That’s not luck-it’s science. Terbinafine kills the fungus instead of just slowing it down.
Prevention: The Real Secret to Staying Fungus-Free
Treatment works-but without prevention, you’re just playing whack-a-mole. Here’s what actually helps:
- Keep feet dry. Moisture between toes is the #1 trigger. Use antifungal powder (like 2% miconazole) daily, especially after showers.
- Change socks daily. Cotton or moisture-wicking fabrics are best. Don’t wear the same pair two days in a row.
- Avoid barefoot walking. Wear flip-flops in public showers, pools, and gyms. Fungi survive for months on damp floors.
- Don’t share towels or shoes. Even if someone looks fine, they might be carrying the fungus.
- Wash shoes. Spraying them with antifungal spray or leaving them in the sun helps kill lingering spores.
- Don’t scratch. Scratching spreads fungus to your hands, groin, or under nails. That’s how jock itch starts.
People with diabetes need extra care. Poor circulation and nerve damage mean they might not feel the early signs of infection. Untreated athlete’s foot can lead to cellulitis-or worse, bone infection. The CDC recommends daily foot checks for diabetics.
What’s New in Antifungal Treatment?
The last big breakthrough was fluconazole in the 1990s. But things are changing. In 2021, the FDA approved Ibrexafungerp, the first new class of antifungal in 20 years. It’s for vaginal yeast infections that don’t respond to standard treatments.
Researchers are also testing olorofim, a new topical drug that cleared 82% of stubborn athlete’s foot cases in Phase II trials in early 2023. It works against strains that resist older drugs.
But the biggest threat? Resistance. A new strain of athlete’s foot fungus, Trichophyton indotineae, was first spotted in India in 2017. Now it’s in 28 countries. It doesn’t respond to terbinafine or clotrimazole. The WHO lists it as a priority pathogen. If this spreads, we could see more treatment failures.
When to See a Doctor
You don’t need to run to the doctor for every itchy toe. But call if:
- The infection doesn’t improve after 2 weeks of OTC treatment.
- You see pus, swelling, red streaks, or fever-signs of a bacterial infection.
- You have diabetes or a weakened immune system.
- The infection keeps coming back.
Doctors can do a skin scraping test to confirm it’s fungal-not eczema or psoriasis. That’s important-misdiagnosis is common.
And yes, you can treat yeast infections at home with fluconazole or clotrimazole suppositories. But if you’ve never had one before, see a doctor first. Other conditions-like bacterial vaginosis or STIs-can mimic yeast symptoms.
Final Takeaway
Fungal infections are annoying, but they’re not mysterious. Athlete’s foot and Candida are different bugs needing different fixes. Topical creams work for mild cases-but only if you use them long enough. Oral meds are faster and more reliable for stubborn or recurring infections.
The real win? Prevention. Dry feet. Clean socks. No barefoot walking. These simple habits cut your risk by 80%. And if you’ve been stuck in a cycle of treatment and relapse, it’s not you-it’s the treatment plan. Switch to terbinafine. Finish the full course. Stop scratching. You don’t need to live with it.
Can athlete’s foot spread to other parts of the body?
Yes. Scratching or touching the infected area and then touching other parts of your body can spread the fungus. That’s how jock itch or fungal nail infections often start. Always wash your hands after applying cream or touching your feet.
Is athlete’s foot contagious?
It’s mildly contagious. You don’t need to be in direct contact with someone to catch it. Fungal spores shed from skin can live on floors, towels, and shoes for weeks. Walking barefoot in public showers is the most common way people get infected.
Can I use the same antifungal cream for both athlete’s foot and a yeast infection?
Some creams, like clotrimazole, work for both. But terbinafine is only for dermatophyte infections like athlete’s foot. For vaginal yeast infections, fluconazole or vaginal suppositories are more effective. Don’t guess-check the label or ask a pharmacist.
Why does my athlete’s foot keep coming back?
Most people stop treatment too soon. Even if the itching is gone, the fungus is still alive. You need to keep using the cream for 1-2 weeks after symptoms disappear. Also, if you’re not keeping your feet dry or wearing the same shoes, you’re re-exposing yourself.
Are natural remedies like tea tree oil effective?
Some studies show tea tree oil has antifungal properties, but it’s not reliable. The concentration in store-bought oils varies, and there’s no standard dosage. For a serious infection, stick to FDA-approved antifungals. Natural doesn’t mean safe or effective.
Can I treat fungal nail infections with the same creams as athlete’s foot?
Topical creams usually don’t penetrate thick nails. Oral antifungals like terbinafine or itraconazole are needed for nail infections. Treatment can take 3-12 months, depending on how fast your nails grow. Patience is key.
How do I know if it’s a yeast infection or bacterial vaginosis?
Yeast infections cause thick, white, cottage cheese-like discharge and intense itching. Bacterial vaginosis has a thin, grayish discharge with a fishy odor, especially after sex. BV doesn’t usually itch. If you’re unsure, see a doctor-self-treating the wrong condition can make it worse.
Do antifungal pills hurt your liver?
Oral antifungals like terbinafine and itraconazole can affect liver enzymes, but serious damage is rare. Your doctor will check your liver function before and during treatment, especially if you’re on it for more than 2 weeks. Don’t drink alcohol while taking these meds.


Write a comment