Bisphosphonate Timing Calculator
This tool helps you determine the safe timing for taking your bisphosphonate medication and when you can safely consume food, drinks, or other medications that might interfere with absorption. Based on medical guidelines from the FDA and clinical studies.
Recommended timing:
Critical Reminder
Even 30 minutes is the minimum. For best results, wait 60 minutes before eating or drinking anything other than plain water.
Take your osteoporosis pill with milk. It seems harmless. Maybe even helpful. After all, milk has calcium-your bones need calcium, right? But if you’re on a bisphosphonate like alendronate (Fosamax) or risedronate (Actonel), that glass of milk could be ruining your treatment before it even starts.
Why Your Pill Stops Working
Bisphosphonates are powerful drugs designed to slow bone loss and prevent fractures. They work by shutting down the cells that break down bone. For people with osteoporosis, this can cut hip fracture risk by nearly half. But here’s the catch: these drugs are absorbed terribly by the body to begin with. Alendronate absorbs at just 0.6% to 0.7%. Risedronate? Barely better-0.6% to 1.0%. That means if you take a 70mg pill, your body might only use half a milligram. The rest? Gone. And dairy? It makes it worse. Milk, cheese, yogurt, even fortified plant-based milks-they’re packed with calcium, magnesium, and other minerals. These minerals latch onto bisphosphonates in your stomach and gut, forming a chemical bond that your body can’t break. The result? Up to 90% of your dose gets trapped and flushed out. Studies show that eating just 30 grams of cheese-about the size of a golf ball-can block nearly all absorption of a 100mg risedronate pill. The FDA’s own prescribing info for Fosamax says this plainly: "Absorption of alendronate is reduced when administered with or immediately after a meal, and is markedly decreased in the presence of calcium." It’s not a suggestion. It’s a warning built into the science.The Exact Rules You Can’t Ignore
There’s no wiggle room. No "I’ll just wait 15 minutes." No "I had a sip of coffee earlier." The guidelines are strict for a reason:- Take your pill first thing in the morning, before eating or drinking anything else.
- Use plain water-only 6 to 8 ounces. No sparkling, no mineral, no orange juice.
- Stay upright (sitting or standing) for at least 30 minutes after taking it. Lying down increases the risk of the pill getting stuck in your esophagus.
- Wait 30 to 60 minutes before eating, drinking, or taking any other medication-including calcium supplements, antacids, or iron pills.
Dairy Isn’t the Only Culprit
You might think it’s just milk and cheese. But it’s not. Anything with calcium, iron, magnesium, or aluminum can interfere:- Fortified plant milks (almond, soy, oat)-many have added calcium equal to dairy.
- Orange juice-even if it’s not fortified, the citric acid and minerals lower absorption by 50-60%.
- Coffee and tea-caffeine isn’t the issue, but the minerals and compounds in them bind to the drug.
- Bran cereal-high in fiber and phytates, which also block absorption.
- Antacids and calcium supplements-even if taken hours later, they can still interfere if taken too close.
Why People Keep Getting It Wrong
It’s not laziness. It’s confusion. People don’t realize how sensitive these drugs are. One Reddit user shared: "I took my Fosamax with orange juice for three months. My bone density scan showed zero improvement." Another said: "I thought yogurt was good for bones, so I ate it right after my pill. My doctor was furious." The National Osteoporosis Foundation’s 2022 patient survey found that 41% of bisphosphonate users found the rules "very difficult" to follow. For people over 65, that number jumped to 53%. Morning nausea, memory issues, or just being in a rush-these things make perfect adherence impossible. And yet, the consequences are real. A 2022 study in PMC9029784 showed that patients who took their pill with food had no measurable improvement in bone density. The drug simply didn’t work. That means someone might be paying $4 a month for a pill that’s doing nothing.Real Solutions People Actually Use
People who stick with it don’t just follow rules-they build systems:- Keep a glass of water and your pill on your nightstand. Take it right when you wake up.
- Set a phone alarm: "Take pill." Then another: "Wait 30 min."
- Use a pillbox labeled "Bisphosphonate Only"-separate from your vitamins.
- Delay coffee until after 30 minutes. If you need caffeine, try herbal tea after the window.
- Choose oat milk or almond milk that’s unfortified for your morning cereal.
- Keep a log: "Took pill at 6:00am. Ate at 6:32am. No dairy."
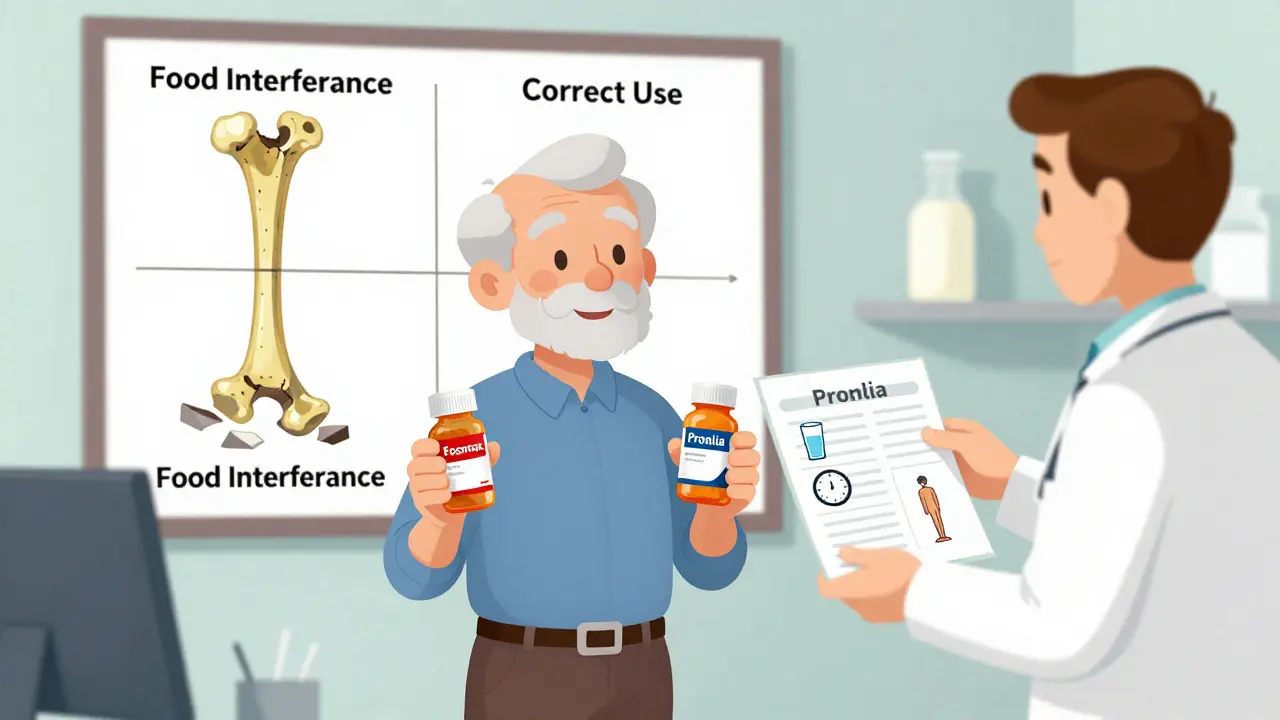
Alternatives If You Can’t Stick to the Rules
If you’ve tried and failed-multiple times-you’re not alone. And you don’t have to suffer. Injectable options exist:- Denosumab (Prolia): A shot every six months. No food restrictions.
- Teriparatide (Forteo): Daily injection for up to two years. Boosts bone formation, not just slows loss.


Write a comment