If you take a calcium channel blocker for high blood pressure or chest pain, eating a grapefruit or drinking a glass of grapefruit juice might seem harmless - but it could be putting you at serious risk. This isn’t just a myth or a vague warning. It’s a well-documented, potentially life-threatening interaction that affects millions of people worldwide. The problem isn’t with the medication itself - it’s with what happens when citrus, especially grapefruit, meets your pills.
Why Grapefruit Is a Problem
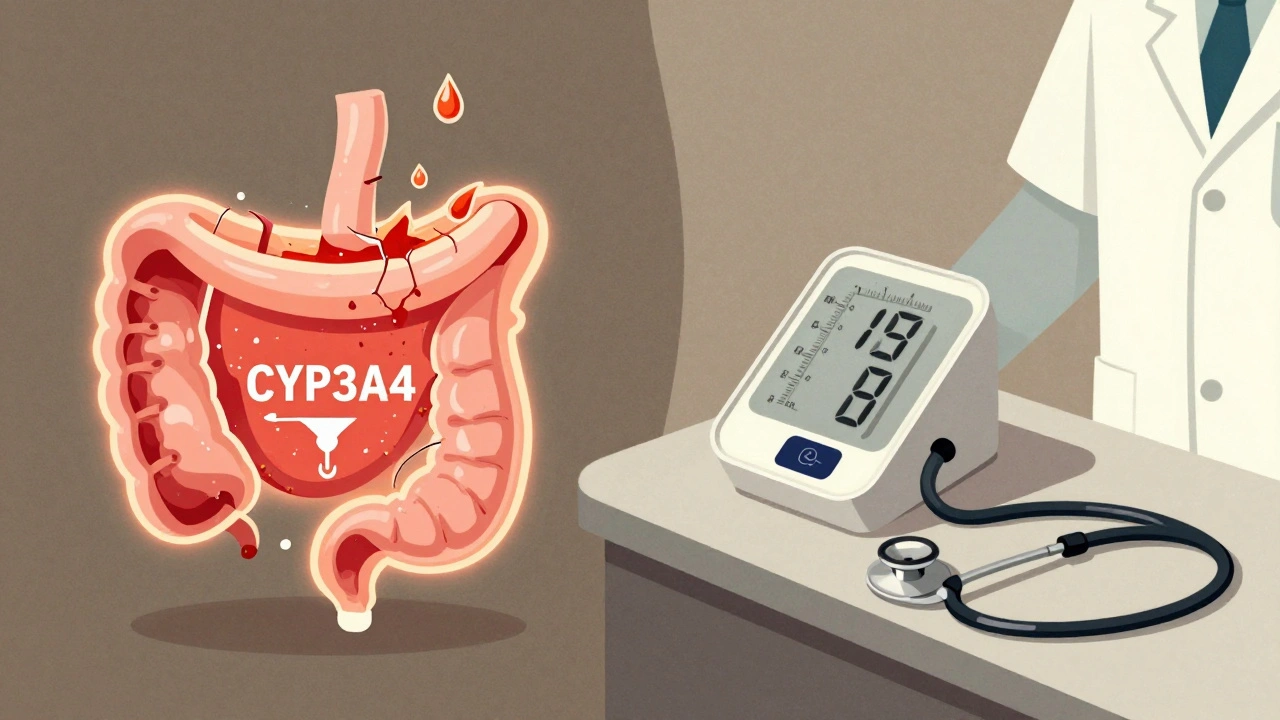
Grapefruit doesn’t just taste tart - it contains chemicals called furanocoumarins, specifically 6’,7’-dihydroxybergamottin and bergamottin. These compounds shut down an enzyme in your gut called CYP3A4. That enzyme normally breaks down certain drugs before they enter your bloodstream. When it’s blocked, your body absorbs way more of the drug than it should. For calcium channel blockers like felodipine, nimodipine, and nicardipine, this means your blood levels can jump by 300% to 500%. One 200ml glass of grapefruit juice - about one cup - is enough to cause this effect. And it doesn’t matter if you take your pill hours later. The enzyme stays turned off for up to 72 hours. So even if you drink grapefruit juice in the morning and take your blood pressure pill at night, you’re still at risk.Which Calcium Channel Blockers Are Most Affected?
Not all calcium channel blockers react the same way. The ones most at risk are the dihydropyridine types:- Felodipine - The worst offender. Grapefruit can boost its levels by up to 5 times.
- Nimodipine - Used for brain blood flow after stroke; interaction can lead to dangerous drops in blood pressure.
- Nicardipine - Also significantly affected.
- Pranidipine - Less common, but still risky.
Amlodipine (Norvasc) is often considered safer, but studies show it still interacts - just less dramatically. Some experts say it’s a better choice if you want to keep eating citrus, but it’s not risk-free.
On the other hand, non-dihydropyridine blockers like verapamil and diltiazem have weaker interactions. That doesn’t mean they’re safe - just that the risk is lower. Still, no one should assume they’re immune.
What Happens When You Mix Them?
When too much calcium channel blocker enters your system, your blood pressure can crash. Symptoms include:- Severe dizziness or lightheadedness
- Extreme fatigue
- Flushing or warm skin
- Swelling in the ankles or legs
- Rapid or irregular heartbeat
- Fainting or near-fainting episodes
These aren’t just uncomfortable - they’re dangerous. In older adults, even a small increase in drug levels can make standing up unsafe. One nurse practitioner described a case where an elderly patient collapsed after eating grapefruit with her morning dose of felodipine. She ended up in the ER with dangerously low blood pressure.
What makes this worse is that many people don’t realize they’re at risk. A 2022 survey found that 68% of patients taking calcium channel blockers had never heard of this interaction. Even worse, only 37% of primary care doctors routinely ask their patients about grapefruit consumption.
What About Other Citrus Fruits?
Not all citrus is created equal. Grapefruit is the worst because it has the highest concentration of furanocoumarins - up to 10 mg per 100ml. Other citrus fruits? Not so much.- Seville oranges (sour oranges used in marmalade) - Also contain furanocoumarins. Avoid.
- Tangelos (a grapefruit-orange hybrid) - Same risk as grapefruit.
- Regular sweet oranges (like Valencia or Navel) - Safe. They have negligible levels of the harmful compounds.
- Clementines, mandarins, tangerines - Also safe.
- Lemons and limes - Minimal risk. No significant interaction reported.
So yes - you can still enjoy your morning orange juice. Just avoid anything labeled “grapefruit,” “Seville orange,” or “tangelo.”
What Should You Do Instead?
If you’re on a calcium channel blocker and you love citrus, here’s what to do:- Check your prescription label. Felodipine, nimodipine, and nicardipine come with black box warnings about grapefruit. If yours does, avoid it completely.
- Ask your pharmacist or doctor. Don’t assume your medication is safe. Ask specifically: “Does this interact with grapefruit?”
- Switch to a safer alternative. If you really want to keep citrus in your diet, talk to your doctor about switching to a blood pressure medication that doesn’t interact. ACE inhibitors like lisinopril, ARBs like valsartan, thiazide diuretics like hydrochlorothiazide, and beta blockers like metoprolol are all safe options.
- Read labels on packaged juices. Some “citrus blends” contain grapefruit juice even if it’s not obvious. Look for “grapefruit juice” on the ingredient list.
- Wait 72 hours. If you accidentally ate grapefruit, don’t take your next dose until three full days have passed. Don’t just wait until tomorrow.

Why This Interaction Is Still a Hidden Danger
You’d think this would be common knowledge by now. After all, it was first documented in 1989. But it’s not. Many patients still eat grapefruit without realizing the risk. Clinicians still don’t ask. Pharmacies still don’t warn.Here’s the hard truth: an estimated 15,000 emergency room visits in the U.S. each year are linked to grapefruit-drug interactions - and calcium channel blockers are among the top culprits. That’s not a small number. It’s preventable.
Researchers are working on solutions. Two new extended-release versions of amlodipine are in late-stage trials and show a 70% reduction in grapefruit interaction. But those aren’t on the market yet.
Until then, the only reliable solution is avoidance - and awareness.
Final Advice
If you take a calcium channel blocker:- Don’t eat grapefruit. Don’t drink grapefruit juice. Don’t even try to time it around your dose.
- Don’t assume your orange juice is safe if it’s labeled “citrus blend.”
- Ask your doctor if you can switch to a medication that doesn’t interact.
- Tell your family - especially older relatives - because they’re at highest risk.
- If you feel dizzy, faint, or your heart races after eating citrus, seek medical help.
This isn’t about being overly cautious. It’s about survival. One grapefruit can turn a safe dose into a toxic one. That’s not a guess - it’s science. And it’s happening every day to people who had no idea.
Can I drink orange juice with my calcium channel blocker?
Yes - regular sweet oranges like Valencia or Navel are safe. They don’t contain enough furanocoumarins to interfere with your medication. But avoid Seville oranges and tangelos, which are hybrids with grapefruit and carry the same risk.
How long does the grapefruit interaction last?
The enzyme-blocking effect lasts up to 72 hours. Even one glass of grapefruit juice can shut down CYP3A4 in your gut for three days. That means taking your pill the next morning won’t help - the interaction is still active.
Is amlodipine safe with grapefruit?
Amlodipine has a weaker interaction compared to felodipine or nimodipine, but it’s not zero. Some studies show a 20-30% increase in blood levels. If you’re concerned, ask your doctor if switching to a non-interacting medication like lisinopril or metoprolol is an option.
What should I do if I accidentally ate grapefruit with my medication?
Don’t panic, but monitor yourself. Watch for dizziness, fainting, swelling, or an unusually fast heartbeat. If you feel any of these, call your doctor or go to urgent care. Avoid grapefruit for the next 72 hours and don’t take another dose until then.
Why don’t more doctors warn patients about this?
Studies show most doctors don’t routinely ask about grapefruit use. It’s an oversight - not because they don’t know, but because it’s easy to forget in a busy clinic. That’s why it’s critical that you ask first. Don’t wait for your doctor to bring it up.
Are there any new medications that won’t interact with grapefruit?
Yes - two new extended-release versions of amlodipine are in Phase III clinical trials and show a 70% reduction in grapefruit interaction. They’re not available yet, but they represent a promising step forward. For now, avoidance and switching to non-interacting drugs are your best options.


Write a comment