Blood Thinner Bleeding Emergency Checker
Check Your Symptoms
Select your symptoms to determine if you need emergency care. Based on medical guidelines for anticoagulant users.
Taking a blood thinner can save your life - but it also means your body is one cut, bump, or fall away from serious trouble. If you’re on warfarin, Eliquis, Xarelto, Pradaxa, or any other anticoagulant, you’ve probably worried about bleeding. You’re not alone. About 3% of people on these meds have a major bleeding event each year. Most of the time, it’s manageable. But sometimes, it’s an emergency. Knowing the difference could mean the difference between a trip to the doctor and a trip to the ER - or worse.
What Counts as a Real Emergency?
Not all bleeding is dangerous. A little oozing from a cut, a quick nosebleed, or even a small bruise? Those are common. But when bleeding doesn’t stop, or it happens inside your body, you need help fast.Go to the emergency room immediately if you have:
- Any bleeding that won’t stop after 10-15 minutes of firm, continuous pressure
- Vomiting blood - bright red or like coffee grounds
- Coughing up blood
- Blood in your urine - pink, red, or brown
- Black, tarry, or sticky stools - this means bleeding in your gut
- A sudden, severe headache, confusion, or loss of consciousness - could be bleeding in the brain
- Severe back or abdominal pain - could signal internal bleeding behind the abdomen
- Difficulty breathing, chest pain, or dizziness when standing - signs your body is losing too much blood
- A head injury, even if you feel fine - intracranial bleeding can take hours to show symptoms
These aren’t just "better safe than sorry" situations. They’re life-threatening. Internal bleeding can cause shock in as little as 30 minutes. The longer you wait, the harder it is to fix.
What’s Just a Nuisance?
Most bleeding episodes on blood thinners aren’t emergencies. In fact, over half of ER visits by people on anticoagulants are for things like nosebleeds, minor cuts, or bleeding gums - problems that can be handled at home.Here’s what’s usually okay:
- A nosebleed that stops after 10-15 minutes of pinching the soft part of your nose
- A small cut that bleeds longer than normal but stops with pressure
- Bleeding gums when brushing - common, but don’t ignore it
- A bruise that’s bigger than usual but doesn’t hurt or swell
- Light spotting between periods - if it’s not soaking through a pad every hour
Still, don’t assume it’s harmless. If you’re unsure, call your doctor or pharmacist. Many clinics now offer telehealth triage for anticoagulant patients. Studies show that 73% of these visits could have been handled over the phone, saving you time and keeping your medication on track.
Why Stopping Your Blood Thinner Is Dangerous
It’s tempting. You get a nosebleed. You’re scared. So you skip your pill. Big mistake.When you stop a blood thinner, your risk of a clot jumps fast. Within 24-48 hours, your blood starts clotting normally again. That’s fine - unless you have atrial fibrillation, a mechanical heart valve, or a history of deep vein thrombosis. Then, your body is a ticking time bomb.
Research from the Michigan Anticoagulation Quality Improvement Initiative found that 68% of patients who stopped their blood thinner after minor bleeding had a clot within 30 days. One man on Reddit shared: "I stopped my pill after a bad cut. Two weeks later, I had a pulmonary embolism. Don’t be like me."
Even a single missed dose can raise your stroke risk by 300% in the first week. That’s not an exaggeration. That’s from the European Heart Journal.
Your doctor knows your risk. Never adjust your dose or stop the medication without talking to them first.
How to Handle Minor Bleeding at Home
If you’re sure it’s not an emergency, here’s what works:For cuts:
- Apply firm, direct pressure with a clean cloth or gauze - no peeking.
- Keep pressure going for at least 10 minutes. (Most people check too soon.)
- Elevate the injury above your heart if possible.
- Don’t use hydrogen peroxide or alcohol - they slow healing.
- Once it stops, cover with a bandage.
For nosebleeds:
- Sit upright and lean slightly forward - don’t tilt your head back.
- Pinch the soft part of your nose (just below the bridge) for 10-15 minutes.
- Use a cold pack on the bridge of your nose if you have one.
- If it’s still bleeding after 30 minutes, call 911 or go to the ER.
For gums:
- Use a soft-bristled toothbrush.
- Rinse with salt water.
- Ask your dentist if you need to adjust your oral care routine.
These steps cut down on unnecessary ER visits. Patients who get proper home management education reduce ER trips by 41% and stick to their meds better.
How Blood Thinners Differ - And Why It Matters
Not all blood thinners are the same. The older one, warfarin, needs regular blood tests and has lots of food and drug interactions. Newer ones - called DOACs (direct oral anticoagulants) - like Eliquis, Xarelto, and Pradaxa, don’t need testing and have fewer interactions.But they also have different bleeding risks:
| Medication | Major Bleeding Risk |
|---|---|
| Warfarin | 3.77 |
| Dabigatran (Pradaxa) | 3.21 |
| Rivaroxaban (Xarelto) | 3.60 |
| Apixaban (Eliquis) | 2.13 |
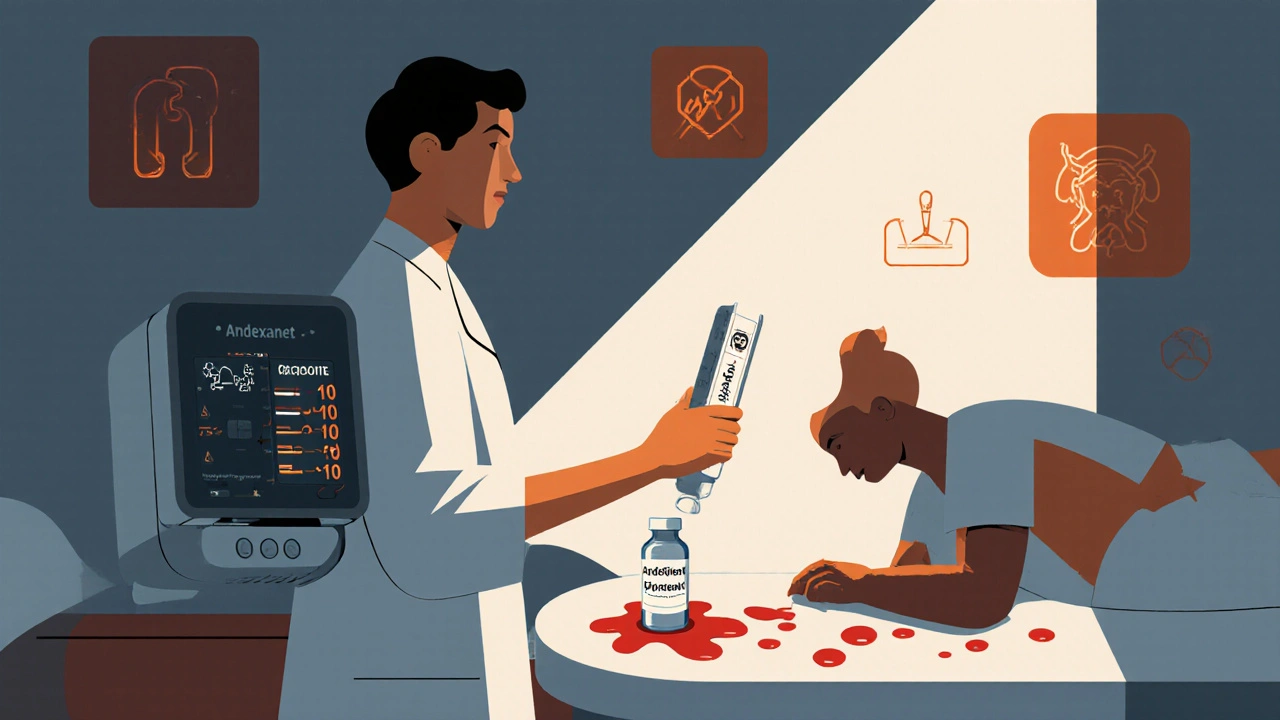
Apixaban has the lowest bleeding risk among the common DOACs. If you’ve had bleeding before, your doctor might switch you to it. And if you’re on Xarelto or Eliquis now, there’s a reversal drug - andexanet alfa - that can stop bleeding in under an hour. That wasn’t available five years ago.
What’s Changing in Emergency Care
The field is moving fast. In 2024, a new universal reversal agent called ciraparantag is expected to be approved. It can reverse all types of blood thinners - even the ones that currently don’t have a specific antidote.Emergency rooms are also getting better at testing. Soon, point-of-care coagulation tests will give results in minutes, not hours. That means faster treatment and better outcomes.
Telemedicine is growing too. By 2026, nearly half of all minor bleeding concerns will be handled remotely. That’s good news - fewer ER visits, less stress, and you stay on your lifesaving medication.

But There’s a Problem: Inequality in Care
Not everyone gets the same help. A 2022 study in JAMA Internal Medicine found that Black and Hispanic patients wait 23-28% longer for reversal drugs in the ER than White patients. That delay increases their chance of dying from bleeding by 15%.This isn’t about individual doctors. It’s about systemic gaps in access, triage, and resources. If you’re a patient of color, advocate for yourself. Ask: "Do you have a reversal agent available?" If they say no, insist on transfer to a facility that does.
What You Should Do Today
Don’t wait for an emergency to figure this out.- Get a written bleeding action plan from your doctor - what to do at home, when to call, when to go to the ER.
- Keep a list of your meds, doses, and your doctor’s contact info in your wallet or phone.
- Wear a medical alert bracelet that says "Anticoagulant User."
- Know your INR if you’re on warfarin - and what your target range is.
- Don’t take NSAIDs like ibuprofen or naproxen - they increase bleeding risk. Use acetaminophen instead.
- Ask your pharmacist: "Is there a reversal agent for my medication?" If not, ask if you’re a candidate for a different one.
Living on a blood thinner doesn’t mean living in fear. It means being informed. You’ve already taken the first step by reading this. Now, take the next one: talk to your doctor. Get your plan. Know your signs. Stay alive.
What should I do if I start bleeding and I’m not sure if it’s serious?
Apply firm pressure for 10-15 minutes without checking. If it doesn’t stop, or if you have symptoms like dizziness, chest pain, or confusion, go to the ER. If you’re unsure, call your doctor or pharmacist. Many clinics offer 24/7 triage lines for anticoagulant patients. Don’t wait - but don’t panic either.
Can I still exercise or play sports while on blood thinners?
Yes - but avoid high-risk activities like contact sports, skiing, or rock climbing. Low-impact exercises like walking, swimming, and cycling are safe and encouraged. Always wear protective gear, and let your doctor know your activity level. Staying active reduces your risk of clots, which is the whole point of taking the medication.
Why do I need to avoid certain painkillers?
NSAIDs like ibuprofen, naproxen, and aspirin interfere with platelets and increase bleeding risk. Even occasional use can be dangerous. Stick to acetaminophen (Tylenol) for headaches or muscle pain. Always check with your pharmacist before taking any new medicine - including herbal supplements like ginkgo or garlic, which can also thin your blood.
How long does it take for blood thinners to wear off?
It depends on the drug. Warfarin can take 3-5 days to clear. Apixaban and rivaroxaban clear in about 12-24 hours. But even if the drug is gone, your risk of clotting stays high for 24-48 hours after stopping. Never stop your medication without medical supervision - even if you feel fine.
Should I carry a reversal agent with me?
No - reversal agents like andexanet alfa are only given in hospitals or emergency settings. They’re not available for home use. But you should know which one works for your medication and make sure your local ER has it. Ask your doctor to write that info into your medical plan.
Is it safe to get a tattoo or piercing while on blood thinners?
It’s not recommended. Even with proper aftercare, the risk of prolonged bleeding and infection is higher. If you really want one, talk to your doctor first. They may temporarily adjust your dose or recommend switching to a lower-risk medication for a few days - but only under strict supervision.
What if I fall and hit my head but feel fine?
Go to the ER. Even if you feel okay, bleeding inside the skull can take 24-72 hours to show symptoms. A headache, nausea, or confusion later could mean a life-threatening bleed. Don’t wait. Get a CT scan. It’s a 10-minute test that could save your life.
Can I drink alcohol while on blood thinners?
Moderation is key. One drink a day is usually okay. More than that increases bleeding risk and can interfere with how your liver processes the medication - especially warfarin. If you drink regularly, tell your doctor. They may need to check your INR more often.


Write a comment