Drug Interaction Risk Checker
How Dangerous Is This Combination?
Combining benzodiazepines and opioids significantly increases the risk of respiratory depression, which can lead to slowed breathing, loss of consciousness, and death. This checker estimates your risk based on specific medications and dosages.
Results will appear here...
When you take opioids for pain and benzodiazepines for anxiety, you might think you’re managing two separate problems. But together, these drugs can shut down your breathing-slowly, silently, and sometimes fatally. This isn’t a rare accident. It’s a predictable, well-documented danger that kills thousands every year.
Why This Combination Is So Dangerous
Opioids like oxycodone, hydrocodone, and fentanyl work by binding to mu-opioid receptors in the brainstem. These receptors control how hard and how often you breathe. When activated, they reduce the drive to inhale and prolong the time between breaths. This is called opioid-induced respiratory depression (OIRD). At high doses, it can lead to complete breathing stoppage. Benzodiazepines-drugs like diazepam, alprazolam, and lorazepam-work differently. They boost the effect of GABA, the brain’s main calming chemical. This makes neurons less active, including those in the brainstem that keep your breathing regular. Alone, a normal dose of a benzodiazepine might make you drowsy, but it rarely stops your breathing. But when paired with an opioid? The effect isn’t just added. It’s multiplied. A 2018 study showed that when fentanyl and midazolam were given together, minute ventilation dropped by 78%. Alone, fentanyl cut it by 45%. Midazolam alone? Just 28%. That’s not a 73% increase. That’s a near-total collapse of breathing capacity. The two drugs attack breathing from two different angles, and together, they overwhelm the body’s ability to compensate.The Science Behind the Silence
Research from the National Institute on Drug Abuse (NIDA) and peer-reviewed journals like eLife and PMC8424565 have mapped exactly how this happens. The brainstem has two key areas involved in breathing: the preBötzinger Complex and the Kölliker-Fuse/Parabrachial complex (KF/PB). Opioids mainly target the preBötzinger Complex, which sets the rhythm for inhalation. They silence some of these rhythm-generating neurons, making breaths shallower and less frequent. Meanwhile, benzodiazepines hit the KF/PB region, which controls how long you exhale. This causes longer pauses between breaths. Together, they reduce both the number of breaths and the depth of each one. What’s worse? The body doesn’t fight back. Normally, low oxygen or high carbon dioxide triggers a reflex to breathe harder. But both drugs blunt that reflex. You don’t gasp. You don’t wake up. You just stop breathing-and stay asleep.The Numbers Don’t Lie
The Centers for Disease Control and Prevention (CDC) found that in 2019, benzodiazepines were present in 16% of all opioid overdose deaths. In cases involving illicit opioids like heroin or fentanyl, that number jumped to 22.5%. That means nearly one in four fatal overdoses involved this combination. Patients prescribed both drugs are 10 times more likely to die from an opioid overdose than those taking opioids alone. This isn’t speculation. It’s based on data from over 1.3 million patients in a landmark 2016 JAMA Internal Medicine study. The risk is highest among people aged 45 to 64, often those with chronic pain and anxiety disorders. Between 2004 and 2011, emergency room visits for people mixing these drugs rose by 131%. In 1999, fewer than 0.2 people per 100,000 died from this combination. By 2019, that number was 3.8-up over 1,800%.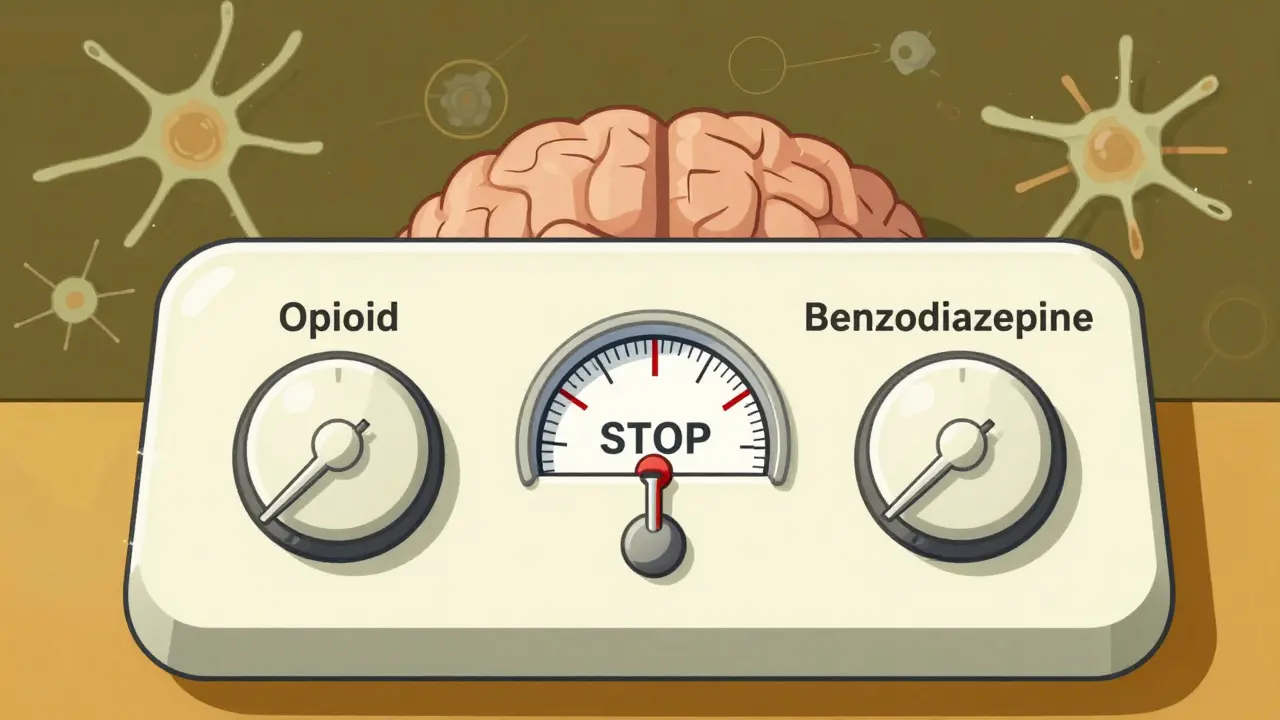
Doctors Know This. So Why Is It Still Happening?
In 2016, the FDA put a black box warning-the strongest possible-on both opioid and benzodiazepine labels. It said: “Concomitant use can result in profound sedation, respiratory depression, coma, and death.” The American Society of Anesthesiologists, the CDC, and the National Institute on Drug Abuse all say the same thing: avoid combining them. Yet, even after the warning, 8.7% of long-term opioid users were still getting benzodiazepines prescribed alongside them in 2022. Why? Because anxiety is real. Pain is real. And many doctors don’t know what else to offer. Some patients were prescribed benzodiazepines years ago for panic attacks or insomnia. When they later needed opioids for back pain or surgery, the benzodiazepine prescription wasn’t reviewed. Others were given both at once because no one thought to question it.What Can Be Done?
The good news? Change is possible. After the FDA’s warning, the rate of concurrent prescribing dropped by 14.5% nationwide. That’s 14.5% fewer people at risk. Here’s what works:- Use non-benzodiazepine options for anxiety. SSRIs like sertraline or escitalopram, or non-addictive anxiolytics like buspirone, are safer long-term choices.
- Try non-opioid pain relief. Physical therapy, nerve blocks, acupuncture, or anti-inflammatories like naproxen can reduce opioid needs.
- Use prescription drug monitoring programs (PDMPs). In 16 states, doctors now get alerts when a patient is prescribed both drugs. These alerts have saved lives.
- Test for drug interactions before prescribing. If you’re on an opioid, ask your doctor if you really need a benzodiazepine. If you’re on a benzodiazepine, ask if opioids are truly necessary.

What If You’re Already Taking Both?
Don’t stop suddenly. Abruptly quitting either drug can cause seizures, severe withdrawal, or rebound anxiety. Talk to your doctor about a plan. If you’re on long-term opioids and benzodiazepines, consider:- Reducing the benzodiazepine dose first, under supervision.
- Switching to a non-addictive sleep aid like trazodone or melatonin if insomnia is the issue.
- Using cognitive behavioral therapy (CBT) for anxiety instead of medication.
- Carrying naloxone. It won’t reverse benzodiazepine effects, but it can save your life if opioids are the main cause of overdose.
What About Reversal? Can Naloxone Help?
Naloxone (Narcan) works fast to reverse opioid overdose. It’s life-saving. But it does nothing for benzodiazepine-induced respiratory depression. If someone overdoses on both, naloxone might restore some breathing-but not enough. The benzodiazepine is still there, still suppressing the brainstem. That’s why some researchers are working on new drugs. A compound called CX1739, tested in animal models in 2022, fully restored breathing after fentanyl and alprazolam were given together. It’s not approved yet, but it shows promise. For now, the best reversal strategy is prevention. Don’t mix them. If you must, use the lowest possible doses for the shortest time. And always have naloxone on hand.The Bottom Line
This isn’t about fear-mongering. It’s about facts. Benzodiazepines and opioids together are a deadly mix. They don’t just increase risk-they multiply it. And the people most at risk? Often, they’re the ones trying to manage real pain and real anxiety. You don’t need to suffer. There are safer ways. Better treatments. Smarter prescriptions. You just need to ask the right questions.If you’re on both, talk to your doctor. If you’re caring for someone who is, learn the signs of overdose: slow, shallow breathing; blue lips; unresponsiveness. Keep naloxone nearby. And never assume someone else’s pain or anxiety justifies the risk.
One breath. That’s all it takes. Don’t gamble with it.
Can you die from taking benzodiazepines and opioids together?
Yes. Combining benzodiazepines and opioids significantly increases the risk of fatal respiratory depression. The CDC reports that in 2019, benzodiazepines were involved in 16% of all opioid overdose deaths. This combination suppresses breathing more than either drug alone, often leading to unconsciousness and stopped breathing without warning.
Does naloxone work on benzodiazepine overdoses?
No. Naloxone only reverses opioid overdoses by blocking opioid receptors. It has no effect on benzodiazepines, which work through GABA receptors. If someone overdoses on both drugs, naloxone may help with the opioid part, but the benzodiazepine will still suppress breathing. Emergency medical care is always needed.
Why do doctors still prescribe these drugs together?
Some doctors prescribe them together out of habit, lack of awareness, or because they believe the patient has no other options. Anxiety and chronic pain often coexist, and benzodiazepines are fast-acting for anxiety. But guidelines from the FDA, CDC, and American Society of Anesthesiologists strongly advise against it. Safer alternatives like SSRIs, CBT, and non-opioid pain treatments exist.
What are safer alternatives to benzodiazepines for anxiety?
SSRIs like sertraline or escitalopram, SNRIs like venlafaxine, and non-addictive anxiolytics like buspirone are safer long-term options. Therapy, especially cognitive behavioral therapy (CBT), is also highly effective. For sleep issues, trazodone or melatonin may help without the risk of respiratory depression.
How can I check if I’m at risk for this interaction?
Review your medications with your pharmacist or doctor. Ask if you’re taking any benzodiazepines (like Xanax, Valium, Klonopin) with opioids (like oxycodone, hydrocodone, fentanyl). Check your state’s prescription drug monitoring program (PDMP) if available. If you’re on both, ask if you can switch to safer alternatives. Never stop either drug suddenly-work with your provider on a taper plan.
Are there any new treatments being developed to reverse this combination?
Yes. Researchers are testing compounds like CX1739, which reversed respiratory depression caused by both fentanyl and alprazolam in animal studies. The NIH’s HEAL Initiative is funding research into drugs that can target both opioid and benzodiazepine effects. Future tools may include wearable breathing stimulators or AI-powered PDMP alerts that flag high-risk prescriptions in real time.
What should I do if someone overdoses on both drugs?
Call 911 immediately. Give naloxone if available-it may help with the opioid component. Perform rescue breathing if the person isn’t breathing. Stay with them until help arrives. Do not leave them alone. Even if naloxone works temporarily, the benzodiazepine effect will return, and breathing can stop again. Medical supervision is critical.


Write a comment