Why most diets fail-and how thinking differently can change everything
You’ve tried the keto diet. The intermittent fasting. The juice cleanses. You lost weight. Then you gained it all back-maybe even more. It’s not your fault. Diets don’t fail because you lack willpower. They fail because they ignore the real problem: your thoughts.
What you eat is only half the story. The other half? What you think about food, your body, and your progress. Behavioral weight loss therapy, especially when rooted in cognitive behavioral therapy (CBT), doesn’t just tell you what to eat. It rewires how you think about eating. And that’s where real, lasting change happens.
How CBT for weight loss actually works
CBT isn’t new. It started in the 1960s as a way to treat depression and anxiety. But in the 1980s, researchers at the University of Pennsylvania noticed something: people struggling with obesity had the same thought patterns as people with depression-negative, rigid, self-critical. So they adapted CBT for weight loss.
Unlike traditional diets that focus on calories and portions, CBT targets the mental habits that sabotage your efforts. It’s not about eating less. It’s about thinking differently so eating less becomes easier.
A 2023 meta-analysis of 9 studies with over 900 participants found that people using CBT lost an average of 1.6 BMI points more than those on standard diets. That might not sound like much, but it’s statistically significant-and it’s sustained. The real win? CBT doesn’t just change your weight. It changes your relationship with food.
The 6 cognitive strategies that make CBT work
Not all therapy is the same. Effective CBT for weight loss uses a specific set of tools, backed by research and tested in clinics. Here are the six that actually move the needle:
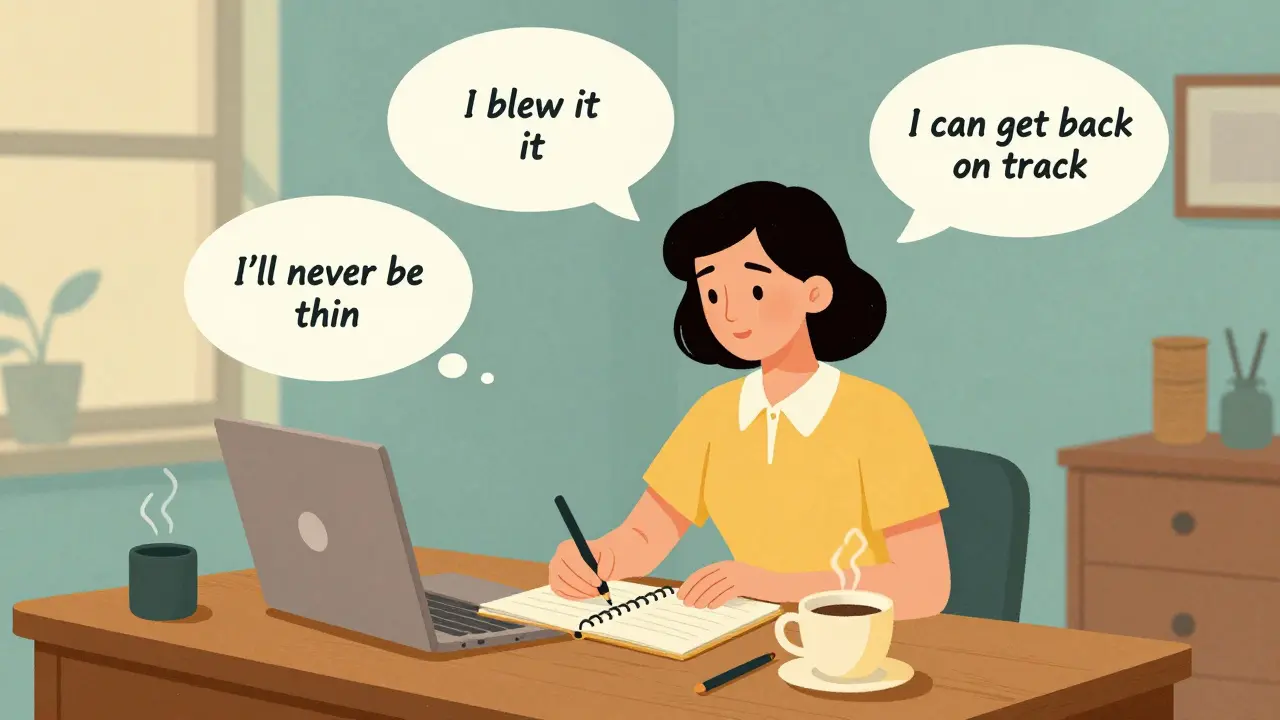
- Cognitive restructuring-This is the core. It’s learning to catch thoughts like “I blew it, I might as well eat the whole cake” and replacing them with “One slip doesn’t define me. I can get back on track now.” Studies show this alone cuts emotional eating by 63%.
- Self-monitoring-Writing down what you eat and how you feel isn’t just busywork. People who track their food and mood consistently lose 5-10% more weight than those who don’t. You don’t need an app. A notebook works. The key is honesty, not perfection.
- Stimulus control-Your environment is your biggest ally or enemy. If your kitchen is full of snacks, your brain will keep reaching for them. CBT teaches you to remove triggers: keep junk food out of the house, don’t eat in front of the TV, use smaller plates. Small changes, big impact.
- SMART goal setting-“Lose weight” is vague. “Lose 1 pound a week by walking 30 minutes, 5 days a week, and eating protein at every meal” is actionable. Specific, measurable, achievable, relevant, time-bound goals keep you focused and give you small wins to build on.
- Problem-solving for high-risk situations-What do you do when you’re stressed? Bored? At a party? CBT doesn’t just tell you to avoid these situations-it gives you a plan. Practice responses ahead of time: “If I’m invited to dessert, I’ll have one bite and savor it, then switch to tea.”
- Relapse prevention-Most people regain weight because they think failure is final. CBT teaches you that setbacks are normal. The goal isn’t to never slip up-it’s to know how to get back on track fast. One mistake doesn’t mean you’ve failed. It means you’re human.

Why face-to-face beats apps-for now
You’ve seen the ads: “Lose weight with AI!” Apps like Noom and WeightWatchers Beyond the Scale use CBT principles. And yes, they help. But here’s the catch: therapist-led CBT leads to 6.8% average weight loss. Apps? Around 3.2%.
Why the gap? Human connection. A real therapist notices when you’re downplaying your progress, challenges your “all-or-nothing” thinking, and adjusts your plan in real time. They don’t just give you a checklist-they build trust.
A 2024 study showed that in-person CBT had 37% higher effectiveness than phone or online-only versions. That’s not because apps are bad. It’s because weight loss isn’t just about behavior. It’s about healing. And healing needs a person.
What CBT doesn’t do-and what it does better than anything else
CBT won’t make you lose 30 pounds in 3 months. It’s not a magic pill. But here’s what it does better than any diet or drug:
- For binge eating disorder (BED): Over half of people with BED stop meeting diagnostic criteria after five years of CBT. That’s not just weight loss-it’s freedom.
- For mental health: Depression and anxiety symptoms drop by 40% in people doing CBT for weight loss-even without direct treatment for those conditions.
- For long-term maintenance: While most people regain 30-35% of lost weight in the first year, those who learned CBT skills keep 2-3 times more weight off long-term.
And here’s the kicker: CBT reduces dropout rates. Standard diet programs lose over half their participants. CBT programs? Only 38.7%. Why? Because it gives people tools to handle the emotional stuff that makes them quit.
The hidden barriers-why CBT isn’t for everyone (yet)
CBT isn’t perfect. And it’s not easy.
First, it takes time. Most programs run 12 to 26 weeks. It takes 8-12 weeks just to learn how to spot and change distorted thoughts. Only 45% of people master cognitive restructuring by week 6 without extra support.
Second, access is limited. In the U.S., there’s only one certified CBT obesity specialist for every 125,000 eligible patients. Rural areas are especially underserved-only 15% of counties have any specialists at all.
Third, insurance rarely covers it. Only 32% of U.S. plans pay for more than 12 sessions. That’s not enough to see real results.
And while CBT alone can help, the best outcomes come when it’s paired with other tools. Motivational Interviewing (MI), for example, boosts weight loss by 50% compared to CBT alone. Why? Because MI helps you find your own reason to change-instead of being told what to do.

What works best: CBT + support
The most powerful approach? Combine CBT with:
- Motivational Interviewing: Helps you connect your weight loss to your values-being strong for your kids, having energy to travel, feeling confident in your skin.
- Nutritional counseling: CBT tells you how to think. Nutrition tells you what to eat. Together, they’re unstoppable.
- Group therapy: A 2022 study showed group CBT delivers nearly the same results as individual sessions-at one-third the cost. You get accountability, shared stories, and the realization that you’re not alone.
And now, even medical treatments like GLP-1 agonists (semaglutide, tirzepatide) are being paired with CBT. Why? Because even the strongest drugs can’t fix the thought patterns that lead to overeating. The NIH just invested $14.7 million in 2024 to test this exact combo. The message? CBT isn’t outdated. It’s essential.
How to get started-even if you’re on a budget
You don’t need a therapist with a PhD to begin. Start here:
- Buy a notebook. Every time you feel the urge to eat when you’re not hungry, write down: What were you feeling? What were you thinking? What happened after?
- Challenge one distorted thought this week. If you think, “I’ll never be thin,” ask: “Is that really true? Have I ever been this stuck before? What’s one small step I could take?”
- Find a free CBT-based app. Apps like Recovery Record or MyFitnessPal (with mood tracking) can help you practice self-monitoring.
- Join a free support group. Organizations like Overeaters Anonymous or online communities focused on CBT principles can offer structure and connection.
You don’t need to do it all. Just start noticing your thoughts. That’s the first step-and the most powerful one.
Final thought: You’re not broken. Your thinking is just out of date.
Weight loss isn’t about discipline. It’s about rewiring. You didn’t fail because you ate the cookies. You failed because your brain told you one mistake meant total failure.
CBT doesn’t promise quick results. But it promises real ones. It gives you the tools to stop fighting yourself-and start working with your mind instead of against it.
The science is clear. The tools exist. The only question left is: Are you ready to change how you think?
Is cognitive behavioral therapy effective for weight loss?
Yes. A 2023 meta-analysis of 9 studies with over 900 participants showed CBT leads to an average BMI reduction of 1.6 points compared to no change in control groups. It’s especially effective for people with binge eating disorder and those struggling with emotional eating. CBT doesn’t just help with weight loss-it improves mental health, reduces anxiety, and builds long-term habits.
How long does CBT for weight loss take to work?
Most programs run 12 to 26 weeks, with weekly sessions. You’ll start noticing changes in your eating habits within 4-6 weeks, but mastering cognitive restructuring-like challenging all-or-nothing thinking-typically takes 8-12 weeks. The real benefits show up after 6 months, when people who learned CBT skills are far more likely to keep weight off than those who only followed a diet.
Can I do CBT for weight loss on my own?
You can start on your own with self-help books, apps, or workbooks, but therapist-led CBT is significantly more effective. Studies show face-to-face CBT produces 37% better results than self-guided versions. The reason? A therapist helps you spot blind spots in your thinking, adjusts your plan, and provides accountability. For best results, combine self-practice with occasional professional guidance.
Does CBT work for people with binge eating disorder?
Yes. In fact, CBT is the most studied and recommended treatment for binge eating disorder. Research shows more than half of people with BED no longer meet diagnostic criteria five years after completing CBT. It helps break the cycle of restriction, bingeing, guilt, and shame by addressing the underlying thoughts that trigger binges.
Why do most people regain weight after losing it?
Most people regain weight because they return to old habits-and old thoughts. Without learning how to handle stress, boredom, or emotional triggers, they fall back into old patterns. CBT teaches you to anticipate these triggers and respond differently. People who use CBT skills are 2-3 times more likely to keep weight off long-term because they’ve changed their relationship with food, not just their diet.
Is CBT covered by insurance?
In the U.S., only 32% of insurance plans cover more than 12 sessions of CBT for weight loss. Many plans don’t cover it at all, or only if you have a diagnosis like BED or depression. Check with your provider. Some employers offer wellness programs that include CBT. Community health centers or university clinics may offer lower-cost options.
What’s the difference between CBT and a diet plan?
A diet plan tells you what to eat and when. CBT tells you why you eat what you do-and how to change that. Diets focus on food. CBT focuses on thought patterns, emotions, and behaviors. You can follow a diet and still binge. You can’t follow CBT without learning to understand your triggers. CBT doesn’t give you a meal plan-it gives you lifelong skills to make better choices, even when no plan is around.

Write a comment