It’s not rare for someone to take an antidepressant and feel better within weeks. But what if that same medication, or a combination of meds, turns dangerous? Serotonin syndrome isn’t something you read about in a textbook-it’s a real, fast-moving medical emergency that can strike within hours. And most people don’t know the signs until it’s too late.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome happens when your body has too much serotonin. It’s not an allergy. It’s not a side effect you can just ‘tough out.’ It’s a toxic overload. This isn’t just about taking too many pills at once. Sometimes, it’s as simple as adding a new medication-like a migraine drug or a cough syrup-and not realizing it interacts with your antidepressant.
Selective serotonin reuptake inhibitors (SSRIs) like fluoxetine, sertraline, and escitalopram are the most common culprits. But so are SNRIs like venlafaxine, MAOIs like phenelzine, and even over-the-counter drugs like dextromethorphan (found in many cough syrups). Painkillers like tramadol and fentanyl can also trigger it. When these mix, your brain and nervous system get flooded. Serotonin, a chemical meant to help you feel calm and happy, starts overstimulating your body.
The first signs? They’re easy to miss. You might think you’re just anxious, or coming down with the flu. But if you’ve recently changed your meds-or added something new-pay attention. This isn’t normal.
The Three Clusters of Symptoms
Serotonin syndrome doesn’t show up as one symptom. It shows up as a trio: mental changes, autonomic chaos, and neuromuscular storms.
Mental status changes include confusion, agitation, restlessness, or even hallucinations. In 78% of cases, people feel mentally off-not just sad or tired, but disoriented. You might not recognize your own thoughts.
Autonomic hyperactivity means your body’s automatic systems go haywire. Your heart races-over 100 beats per minute in 83% of cases. Your blood pressure spikes. You sweat like you’ve run a marathon, even if you’re sitting still. Your pupils dilate to 5-8mm (normal is 2-4mm). You might feel hot, but your skin is clammy. Your breathing gets faster. You could have nausea, vomiting, or diarrhea. In fact, 68% of people with serotonin syndrome vomit, and 63% have diarrhea. That’s not just a stomach bug-it’s a red flag.
Neuromuscular symptoms are the most telling. Tremors? Yes. But more importantly, clonus. That’s when your muscles spasm involuntarily-like your foot jerks when you’re lying down, or your fingers tap uncontrollably. It’s not a tic. It’s not stress. It’s your nerves firing out of control. Clonus is present in 92% of confirmed cases. If you have clonus, you have serotonin syndrome until proven otherwise.
Other signs: muscle rigidity, hyperreflexia (your knee-jerk reflex is way too strong), and twitching. These aren’t subtle. If you’re lying in bed and your leg suddenly jerks up three times in a row, that’s not normal. If your arm feels stiff and won’t move smoothly, that’s not just soreness.
When It Turns Life-Threatening
Most cases are mild and resolve quickly if caught early. But about 30% of cases require hospitalization. And 1 in 10 can be fatal.
Severe serotonin syndrome looks different. Your temperature soars above 38.5°C (101.3°F). In extreme cases, it hits 41.1°C (106°F). That’s not a fever-it’s organ failure waiting to happen. Your muscles lock up. You can’t move. You might have seizures. Your heart rhythm goes wild. You pass out. Your kidneys start shutting down because your muscles are breaking down-a condition called rhabdomyolysis.
Death usually comes from one of two things: uncontrolled high fever, or muscle breakdown flooding your bloodstream with toxins. Both can happen within hours if you ignore the early signs.
How Doctors Diagnose It (And Why You Shouldn’t Wait)
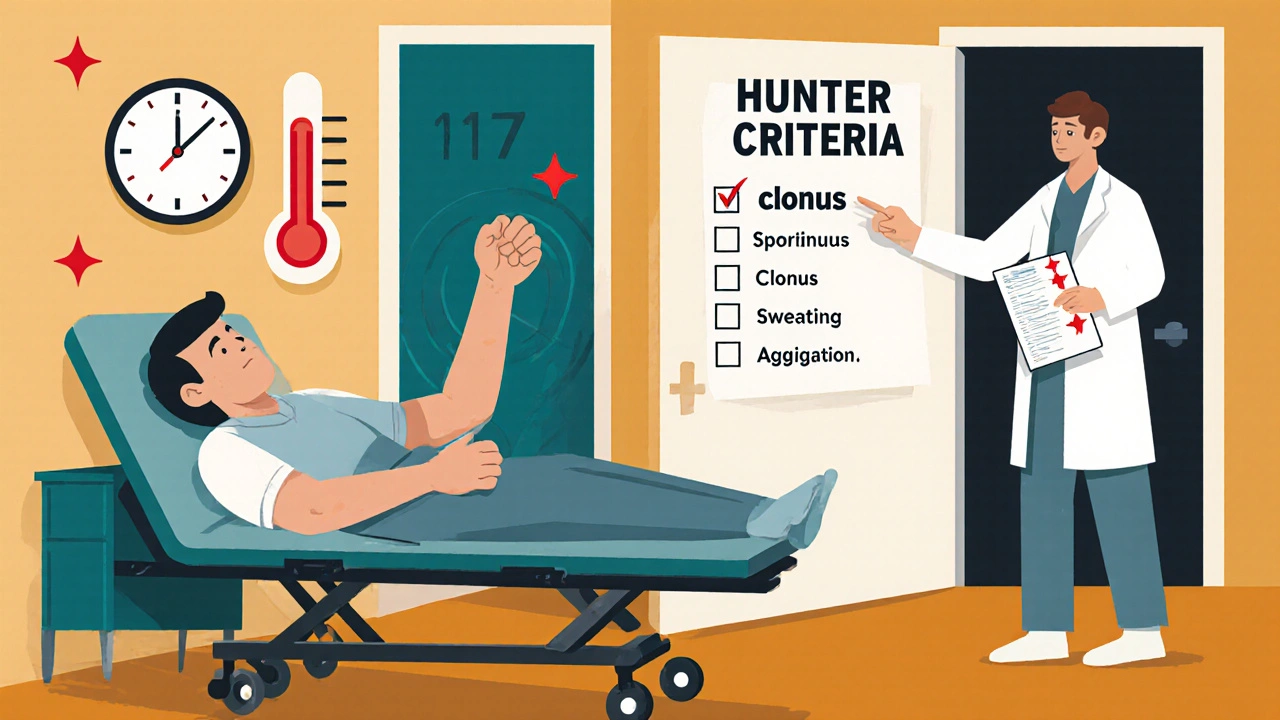
There’s no single blood test that confirms serotonin syndrome. No scan. No X-ray. Diagnosis is based on symptoms and history. The gold standard is the Hunter Serotonin Toxicity Criteria. It’s simple: if you have one of these, you likely have it:
- Spontaneous clonus
- Inducible clonus + agitation or sweating
- Ocular clonus (eye movements) + agitation or sweating
- Tremor + hyperreflexia
- Muscle rigidity + fever + ocular or inducible clonus
This tool is 84% accurate at catching serotonin syndrome and 97% accurate at ruling it out. But here’s the problem: most ER doctors don’t think of it. A 2023 study from the American Psychiatric Association found that 25% of cases are missed. People are sent home with a diagnosis of anxiety, flu, or food poisoning.
That’s why you need to speak up. If you’re on an antidepressant and you feel new tremors, sweating, or muscle jerks after starting a new drug-even something as small as NyQuil-say it. Don’t wait. Don’t assume it’s ‘just stress.’
What to Do If You Suspect Serotonin Syndrome
If you think you or someone else has serotonin syndrome, call emergency services immediately. Don’t wait. Don’t try to ‘sleep it off.’
At the hospital, the first step is simple: stop the medication causing it. Every single one. No exceptions.
Then, they’ll give you:
- Benzodiazepines like lorazepam to calm the nervous system, reduce muscle rigidity, and stop seizures.
- IV fluids to prevent dehydration from vomiting and sweating.
- Cooling measures-ice packs, fans, cool IV fluids-to bring down body temperature slowly and safely.
- Cyproheptadine, the only specific antidote. Given as 12mg orally first, then 2mg every 2 hours until symptoms improve. Most people start feeling better within 24-48 hours if treated fast.
Recovery is possible. Many people feel normal again within 72 hours. But delay? That’s where things turn deadly.
How to Prevent It
Most serotonin syndrome cases happen because of medication interactions. Here’s how to avoid them:
- Never mix antidepressants with other serotonergic drugs without a doctor’s approval. That includes tramadol, fentanyl, triptans (for migraines), dextromethorphan (cough syrup), St. John’s Wort, and even some herbal supplements.
- If switching from an MAOI to an SSRI, wait 14 days. This isn’t optional. It’s a hard rule. The same applies in reverse.
- Keep a full list of everything you take. Not just prescriptions. Include OTC meds, supplements, and even occasional use of cough syrup. Show this to every doctor, even your dentist.
- Ask your pharmacist. They’re trained to spot interactions. If you’re prescribed something new, ask: ‘Can this interact with my antidepressant?’
- Know your risk. If you’ve had serotonin syndrome before, you’re more likely to get it again. Tell every provider.
According to a 2024 study by Cedars-Sinai, patients who received clear warnings about drug interactions were 47% less likely to develop serotonin syndrome. Education saves lives.
Why This Is Getting Worse
The number of serotonin syndrome cases has risen 38% between 2015 and 2022. Why? More people are on antidepressants. More people are taking multiple meds for depression, anxiety, chronic pain, and migraines. Polypharmacy-taking three or more interacting drugs-is involved in 78% of cases.
SSRIs cause 62% of cases. SNRIs, 24%. MAOIs, 8%. But the real danger? People don’t know they’re at risk. Reddit threads from people who survived serotonin syndrome are full of stories like: ‘I was told it was anxiety.’ ‘No one warned me about the cough syrup.’ ‘I thought the shaking was just nerves.’
It’s not your fault. But it’s your responsibility to learn the signs.
Final Warning
Serotonin syndrome doesn’t wait. It doesn’t ask permission. It doesn’t care if you’re ‘just a little anxious.’ If you’re on an antidepressant and you suddenly feel: tremors, sweating, confusion, or muscle jerks-especially after adding a new drug-get help now.
There’s no shame in asking. There’s no ‘overreacting’ when your life is on the line. The difference between recovery and tragedy is often just a few hours.
Can serotonin syndrome happen from one antidepressant alone?
Yes, but it’s rare. Most cases happen when two or more serotonergic drugs are combined. However, taking a very high dose of a single SSRI or SNRI-especially in someone who’s sensitive or has liver problems-can trigger serotonin syndrome on its own. Always take medication exactly as prescribed.
Is serotonin syndrome the same as neuroleptic malignant syndrome (NMS)?
No. NMS is caused by antipsychotic medications and develops over days or weeks. It causes muscle rigidity, fever, and slow reflexes. Serotonin syndrome develops in hours, causes hyperreflexia and clonus, and is linked to antidepressants and other serotonin-boosting drugs. The treatments are different, so misdiagnosis can be deadly.
Can I take ibuprofen or acetaminophen with my antidepressant?
Yes. Regular pain relievers like ibuprofen and acetaminophen do not increase serotonin levels and are generally safe with antidepressants. But avoid combination cold and flu meds that contain dextromethorphan or other serotonergic ingredients. Always check the label.
How long does serotonin syndrome last?
Mild cases resolve in 24-48 hours after stopping the triggering medication. Severe cases may take up to a week, especially if complications like rhabdomyolysis or organ damage occur. Recovery speed depends entirely on how quickly treatment begins.
Are some antidepressants more likely to cause serotonin syndrome?
Yes. SSRIs like fluoxetine (Prozac) and sertraline (Zoloft) are the most common culprits because they’re widely prescribed. SNRIs like venlafaxine (Effexor) carry higher risk due to their dual action. MAOIs like phenelzine are the most dangerous, especially when combined with other drugs. Always discuss your specific medication’s risk profile with your doctor.
Should I stop my antidepressant if I suspect serotonin syndrome?
Do not stop your medication on your own. Call emergency services immediately. Stopping abruptly can cause withdrawal symptoms or worsen your mental health. Medical professionals will guide you on safely discontinuing the drug while managing symptoms.
Can serotonin syndrome come back after recovery?
Yes, if you’re exposed to the same combination of drugs again. Once you’ve had serotonin syndrome, you’re at higher risk. Always inform every healthcare provider about your history. Avoid any drug that increases serotonin unless under strict supervision.
If you’re on antidepressants, talk to your doctor today about your risk. Ask for a full medication review. Write down every pill, supplement, and OTC product you take. Keep that list with you. Serotonin syndrome is preventable-but only if you know what to look for.


Write a comment