Air Pollution Exposure Calculator
Pollution Exposure Check
Enter current pollution levels to see if they exceed irritation thresholds for your nose
Results
Ever notice your nose suddenly running after a walk downtown or while stuck in traffic? That annoying drip isn’t just a random quirk - it’s often your body reacting to air pollution. In this guide we’ll break down why dirty air makes your nose water, which pollutants are the biggest culprits, how you can protect yourself, and when a simple tissue won’t be enough.
What "air pollution" really means
air pollution refers to a mixture of solid particles, liquid droplets, and gases that linger in the atmosphere and harm health. In North America the most common outdoor pollutants are:
- Particulate Matter (PM2.5) - tiny particles less than 2.5 micrometers that can slip deep into the lungs.
- Nitrogen Dioxide (NO2) - a by‑product of vehicle exhaust and industrial combustion.
- Ozone (O3) - a secondary pollutant formed when sunlight reacts with NO2 and volatile organic compounds.
- Allergens hitch a ride on particles, turning pollution into a double‑hit for sensitive noses.
These substances don’t just stay up high; they settle into the air you breathe every minute of the day.
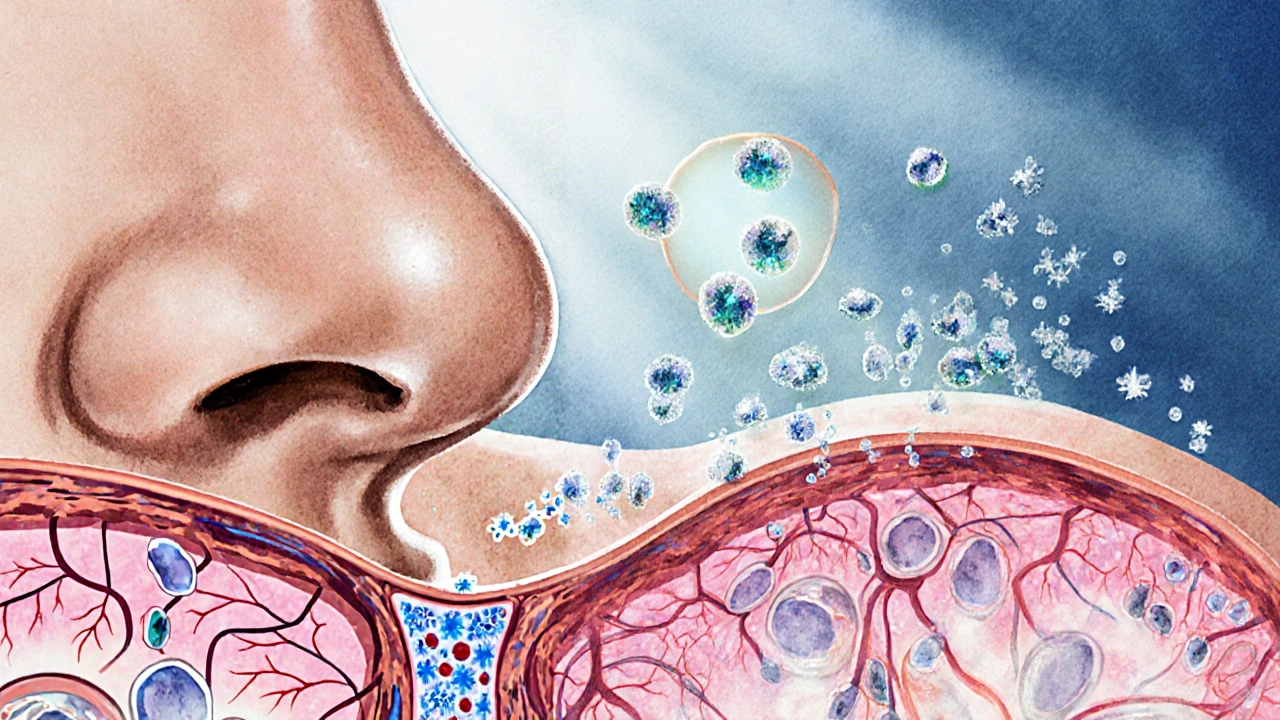
Why a runny nose is the body’s first alarm
The lining of your nasal mucosa is covered in tiny blood vessels and mucus‑producing cells. Its job is to trap dust, microbes, and chemicals, then flush them out. When pollutants irritate these cells, they release histamine and other inflammatory mediators, prompting the glands to pump out extra fluid. The result? A watery, constantly dripping nose.
Unlike a cold, the drip caused by pollution is usually clear, thin, and appears soon after exposure. It often worsens on high‑traffic days, during wildfires, or when temperatures trap smog close to the ground.
Which pollutants trigger the biggest drip?
Not every pollutant affects you the same way. Below is a quick snapshot of the most common offenders and the typical concentration levels that start to cause nasal irritation.
| Pollutant | Typical Urban Level (µg/m³) | Irritation Threshold | Common Sources |
|---|---|---|---|
| PM2.5 | 12‑35 | ≈25µg/m³ | Traffic, heating, wildfires |
| NO2 | 20‑50ppb | ≈40ppb | Cars, diesel generators |
| Ozone (O3) | 30‑70ppb | ≈60ppb | Sunlight‑driven reactions |
When any of these numbers creep above the irritation threshold, expect your nose to start watering, especially if you’re already prone to allergies.
How to keep the drip at bay
Luckily, there are practical steps you can take whether you live in a bustling city like Vancouver or a quieter suburb.
- Check the Air Quality Index (AQI) each morning. Provincial health sites publish real‑time data; aim to schedule outdoor runs when the AQI is ‘Good’ (0‑50).
- Invest in a air purifier with a true HEPA filter for your home. It captures >99.97% of particles down to 0.3µm, cutting indoor PM2.5 dramatically.
- Wear a properly fitted mask (N95 or KN95) on high‑pollution days. Look for a seal that doesn’t leak around the nose - otherwise the mask can actually push polluted air toward your nasal passages.
- Hydrate. Drinking water thins mucus, making it less sticky and easier for the body to clear.
- Consider a saline nasal rinse after exposure. A simple squeeze bottle with sterile saline can wash away trapped particles and reduce inflammation.
These actions don’t eliminate pollution, but they lower the amount that reaches your nasal mucosa, which translates into fewer drips.
When an over‑the‑counter fix helps
If the drip is relentless despite your preventive measures, a short‑term medication may ease the irritation.
- Antihistamines (e.g., cetirizine, loratadine) block histamine receptors, reducing mucus production.
- Topical nasal corticosteroid sprays (fluticasone, budesonide) calm inflammation for chronic sufferers.
- Decongestant drops or pills (pseudoephedrine) can shrink swollen nasal tissue, but should not be used for more than three days in a row.
Always read the label and, if you have underlying conditions like high blood pressure, check with a pharmacist before reaching for a decongestant.

Red flags: When a runny nose signals something more
Most of the time a pollutant‑induced drip is harmless, but certain signs mean you need professional care:
- Persistent nasal discharge lasting more than two weeks.
- Thick, colored mucus (yellow or green) indicating infection.
- Facial pain, fever, or sinus pressure.
- Worsening asthma symptoms or shortness of breath.
If any of these appear, book an appointment with your family doctor or an ear‑nose‑throat (ENT) specialist. Early diagnosis can prevent chronic sinusitis or allergic rhinitis from spiraling.
Bottom line: breathe smarter, not harder
Air pollution is a silent trigger that can turn a clear day into a series of sniffles. By understanding which pollutants matter, monitoring real‑time air quality, and taking a few simple protective steps, you can keep your nose dry and your lungs happy. Remember: the best defense is awareness, followed by a good mask, clean indoor air, and-if needed-an over‑the‑counter antihistamine.
Frequently Asked Questions
Can indoor air quality cause a runny nose too?
Absolutely. Indoor sources like cooking fumes, tobacco smoke, and even scented cleaners release particles that irritate the nasal lining. Using a HEPA‑rated air purifier and keeping windows closed during outdoor smog spikes can dramatically reduce indoor triggers.
Is a standard surgical mask enough to stop a runny nose?
Surgical masks filter larger droplets but let most fine particles (PM2.5) pass through. For noticeable relief, choose an N95/KN95 mask that seals around the nose and filters at least 95% of particles as small as 0.3µm.
Do antihistamines work for pollution‑related drips?
Yes, because pollution triggers histamine release similar to allergies. Non‑sedating antihistamines like cetirizine can reduce mucus production without making you drowsy.
How often should I rinse my sinuses?
A gentle saline rinse once a day is safe for most people. If you’re exposed to high pollution levels, a second rinse in the evening can help clear residual particles.
When should I see a doctor for a runny nose?
If the drip lasts more than two weeks, turns colored, or is accompanied by facial pain, fever, or worsening asthma, schedule a visit. Persistent symptoms may signal sinus infection or chronic rhinitis that need prescription treatment.


Write a comment